Nearly all implantable medical devices, such as pacemakers and neurostimulators, are limited by the capacity of their onboard batteries. To avoid the need for invasive surgery to replace these devices once their batteries run out, scientists have sought to develop implants that can derive power from the body.
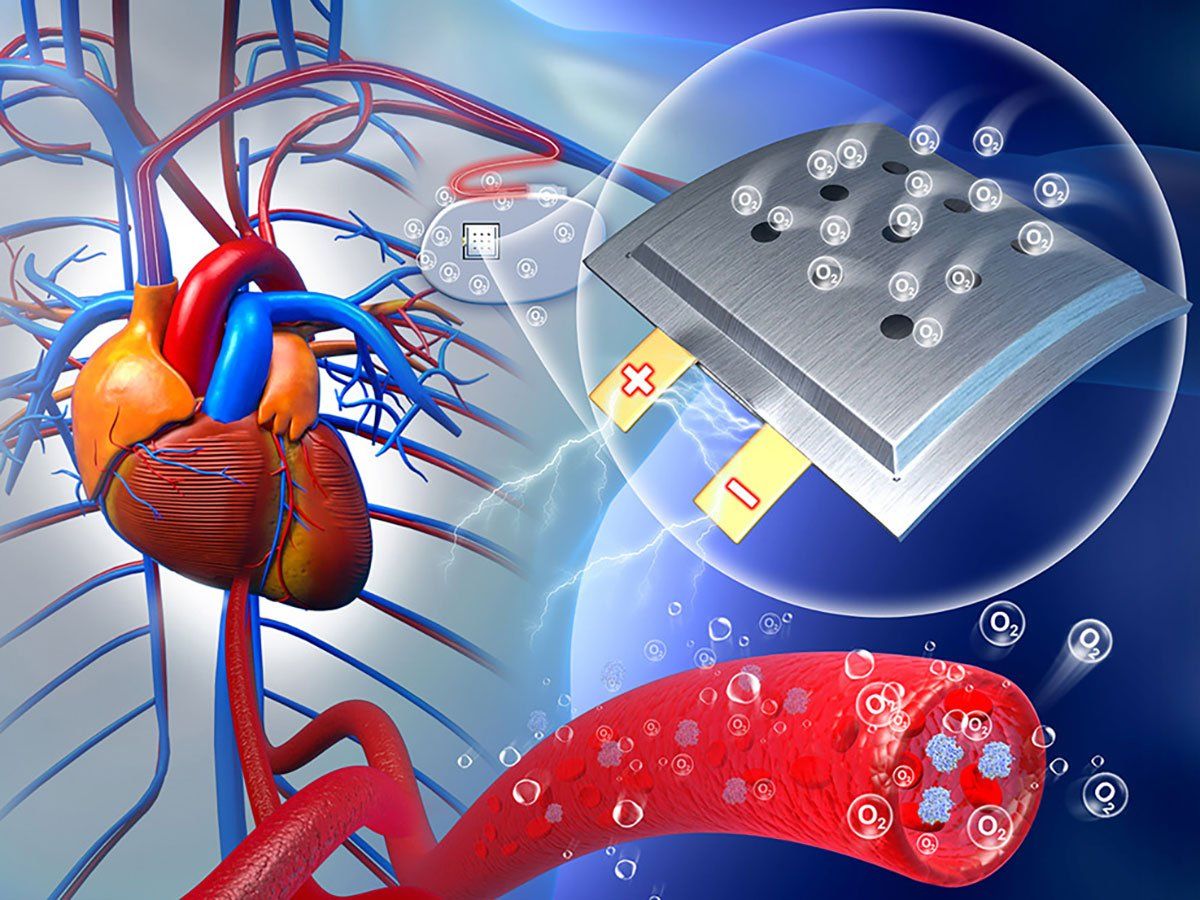
To that end, scientists in China now say they’ve developed a soft, flexible battery that uses oxygen in the blood to help generate electricity—and potentially extend the lifetime of medical implants in the body.
Researchers report that their new battery could extend the service life of implanted devices by three to five times when compared with presently available implantable batteries.
In theory, implanted devices could rely on chemical reactions with oxygen or glucose in the blood for their energy. However, such designs would need to regularly keep electronic components in contact with blood for a continuous energy supply. Developing implants that can perform safely and stably under such conditions has proven challenging.
In a new study, researchers at Tianjin University of Technology in Tianjin, China experimented with electrodes made of a sodium-gallium-tin alloy and nanoporous gold. Sodium is an essential and common element in the human body, and gold is considered a generally biocompatible material. Sodium and gold also have applications in energy—with sodium rechargeable batteries finding use today in stationary energy storage, while nanoporous gold acts like a catalyst and serves as the battery’s cathode.
The scientists packaged their implantable battery in a soft porous flexible polymer film that has previously found use in artificial blood vessels, says Xizheng Liu, a professor of engineering at Tianjin. This protected the electronics while also keeping them in contact with the body’s fluids.
“The battery can run on the continuously supplied oxygen,” Liu says.
The researchers implanted the battery under the skin on the back of rats. They found the device could produce steady voltages of roughly 1.3 volts with a maximum power density of 2.6 microwatts per square centimeter. In comparison, a recent glucose fuel cell achieved less than 0.6 V, but a maximum power density of 43 µW/cm2.
The new battery could operate for at least four weeks, experiencing only a mild decline in performance by the fourth week. The rats healed well after implantation, the scientists report, with the hair on the animals’ backs completely regrown after four weeks, with no obvious inflammation around the devices. The scientists also report that the battery’s chemical byproducts, such as sodium ions, did not appear to affect the kidneys and livers of the rodents. Capillaries regenerated well around the device, providing a continuous source of oxygen for the battery.
Although the prototype battery’s output is not currently enough to power medical devices, the new design reveals it is possible to harvest the body’s oxygen for energy, the researchers say. All in all, the new battery could extend the service life of implanted devices by three to five times when compared with presently available implantable batteries, Liu says.
The scientists say boosting the battery’s performance is also possible—in part via optimizing the efficiency of the nanoporous gold as well as enhancing the flow of ions and oxygen in the device.
The scientists note the battery did show unstable electricity output right after implantation. They found that it needed time for the implantation site to heal, which let blood vessels regenerate around the battery and supply oxygen so it could provide stable electricity. This suggests the battery can also help doctors monitor wound healing, they say.
The researchers add the battery may find applications beyond powering implants. Since tumor cells need oxygen to survive, implanting this oxygen-consuming battery near tumors may help starve cancers, and converting battery energy to heat may also help kill tumor cells, Liu says.
The scientists detailed their findings online 27 March in the journal Chem.
- DARPA Wants Brain Implants That Record From 1 Million Neurons ... ›
- Biodegradable Power Generators Could Power Medical Implants ›
Charles Q. Choi is a science reporter who contributes regularly to IEEE Spectrum. He has written for Scientific American, The New York Times, Wired, and Science, among others.