When 11 University of Chicago researchers reported that they had installed and tested their laser-driven pacemaker in a live animal, their Nature paper laid claim only to “the first minimally invasive optical stimulation of an in vivo pig heart.”
They appear to have achieved more than that.
Together, the team designed, fabricated, and tested what may be the first photovoltaic semiconductor pacemaker. Their approach to the technology could also transform treatments that require stimulating nerves, muscles, or hearts. En route, the Chicago group evaluated photovoltaic materials and developed devices for experiments with cultured heart cells, rodent hearts, in vivo mice and rats, and finally, a sedated adult pig. The device they ultimately developed, for implantation in a pig, was a flexible, two-centimeter square photovoltaic membrane, which was implanted via minimally invasive surgery.
Graduate student Pengju Li says he pulled the multidisciplinary research team together from two Chicago labs—Bozhi Tian’s biology-and-electronics materials group and Narutoshi Hibino’s translational cardiovascular research group.
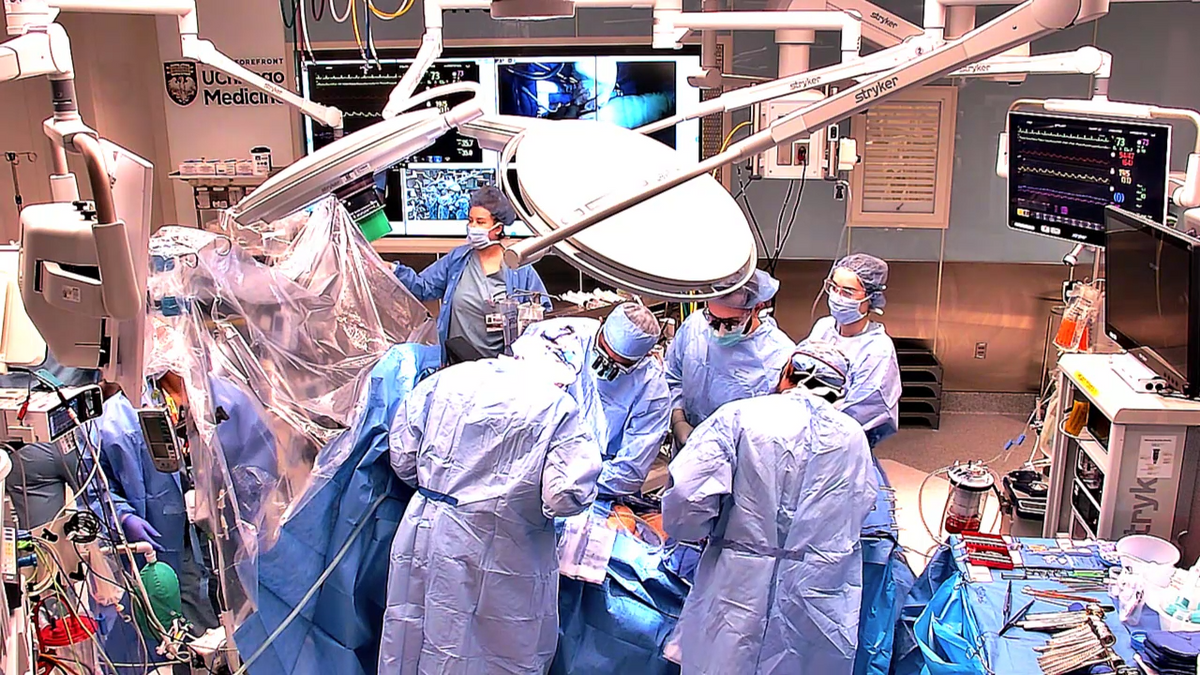
In the culminating experiment, the Chicago surgical team reported in their Nature paper that they inserted the 4-cm2 membrane through a 1-cm slit in the skin between the animal’s ribs. The membrane is thin: the semiconductor layer is just 4 micrometers thick, stabilized on a 21 µm polymer matrix. All but the very finest human hair is thicker. The membrane is also lightweight—around 0.05 grams. Conventional pacemakers, even the new leadless designs (they are “without wires,” not “without element 82”), are 100 to 1000 times heavier.
Consequently, the pacemaker self-adhered to the right ventricle. This natural adhesion is sufficient for short applications in acute treatment, says lab head Bozhi Tian.
Using an endoscope and optical fibers inserted through the same one-centimeter slit, the researchers lit up a selected spot on the pacemaker with a series of one-millisecond laser pulses. (In earlier experiments, they used laser beams as narrow as 10 µm to localize the stimulus.)
The pacemaker overrode the heart’s normal rhythm and accelerated it from 71 to about 120 beats per minute. By moving the beam from one target to another, they also reported they achieved multisite activation—stimulating muscles in both the right and left heart ventricles to produce the kind of contraction patterns that might be needed to return an arrhythmic heart to a normal beat in cardiac resynchronization therapy (CRT).
Tian says the team’s first clinical target will be temporary CRT for patients at risk for sudden cardiac death. CRT in these cases requires brief implantations of a few days to a few months. “CRT definitely requires precise multisite pacing, and we are aiming to apply it to this clinical application first,” Tian says.
Leadless and Minimally Invasive
Conventional pacemakers’ leads are often threaded through a major vein and into one of the heart’s chambers, where the electrode contacts the heart wall. The pacemaker electronics and battery are tucked into a pocket under the skin of the upper chest and attached to the ends of the leads outside the heart.
Leads can, however, sometimes obstruct the veins, interfere with heart valves, or irritate tissues inside the heart—sometimes with serious or even fatal results.
Leadless pacemakers, on the drawing boards since the 1970s, reached the market and clinic in 2014. These are small, self-contained packages, combining very-long-life batteries and pacing electronics. The tiny cylinders weigh just a few grams and are 3 to 4 cm long—somewhere between an AAA battery and a large vitamin capsule in size and shape. Like conventional pacemakers, they are inserted into the heart, threaded through a major vein into a ventricle.
The Chicago design, on the other hand, adheres to the outside of the heart, what’s called the epicardial surface. Nothing is inserted into the heart’s chambers, and nothing is stuck into the external heart muscle. The prototype the Chicago team develop did, they say, require the 1-cm incision in the skin and a 2-cm window in the pericardium (the sac surrounding the heart) for setting the pacemaker and admitting the fiber optic bundle to deliver laser light. And in the prototype, the laser is externally powered. These are challenges to address, the team says, during development.
Li and Tian also say they developed their minimally invasive implantation approach to reduce stress on the subject and promote recovery. “Perhaps, the most fulfilling aspect for me is the initial design of the minimally invasive surgery tool,” Tian says. He says he was inspired by watching an orthopedic surgeon insert polymer implants to repair a torn rotator cuff.
The Heart of the Pacemaker
To build their pacemaker, the Chicago team would need material with a specific set of properties. It would have to produce enough current to stimulate the heart, and the current would have to be highly localized in time and space. To find their best candidate, Li, Tian and their colleagues say they turned to solar cells, testing out a range of alternatives including non-crystalline silicon and single-crystal silicon. The semiconductor they used—a nanoporous single-crystal silicon type—yielded tightly constrained currents in both time and space, the researchers say.
Since then, Tian says, “Pengju has significantly expanded this system to include porous/nanoporous silicon heterojunctions created by other synthetic methods.”
By now, Tian says, “The fabrication process is super-easy. Specifically, the etching process that yields the nanoporous structure takes only about a minute or less in a solution. I believe this makes scalable and low-cost fabrication feasible.”
Igor Efimov, professor of biomedical engineering at Northwestern University in Chicago, wrote in a commentary accompanying the Nature paper that the development offers “exciting proof of concept shows the enormous potential that the technology holds, and suggests that photoelectric devices could eventually transform a range of therapies, including those requiring neural, muscular and cardiac stimulation.”
- How Brain Pacemakers Treat Parkinson’s Disease ›
- No More Invasive Surgery—This Pacemaker Dissolves Instead ›
Douglas McCormick is a freelance science writer and recovering entrepreneur. He has been chief editor of Nature Biotechnology, Pharmaceutical Technology, and Biotechniques.