Implantable medical devices usually have to trade smarts for size. Pacemakers and other active devices with processors on board are typically about a cubic centimeter in size, and must be implanted surgically. Smaller implantable electronics tend to be passive, lacking computing smarts and the ability to actively broadcast signals, says David Blaauw, a professor of electrical engineer and computer science at the University of Michigan in Ann Arbor.
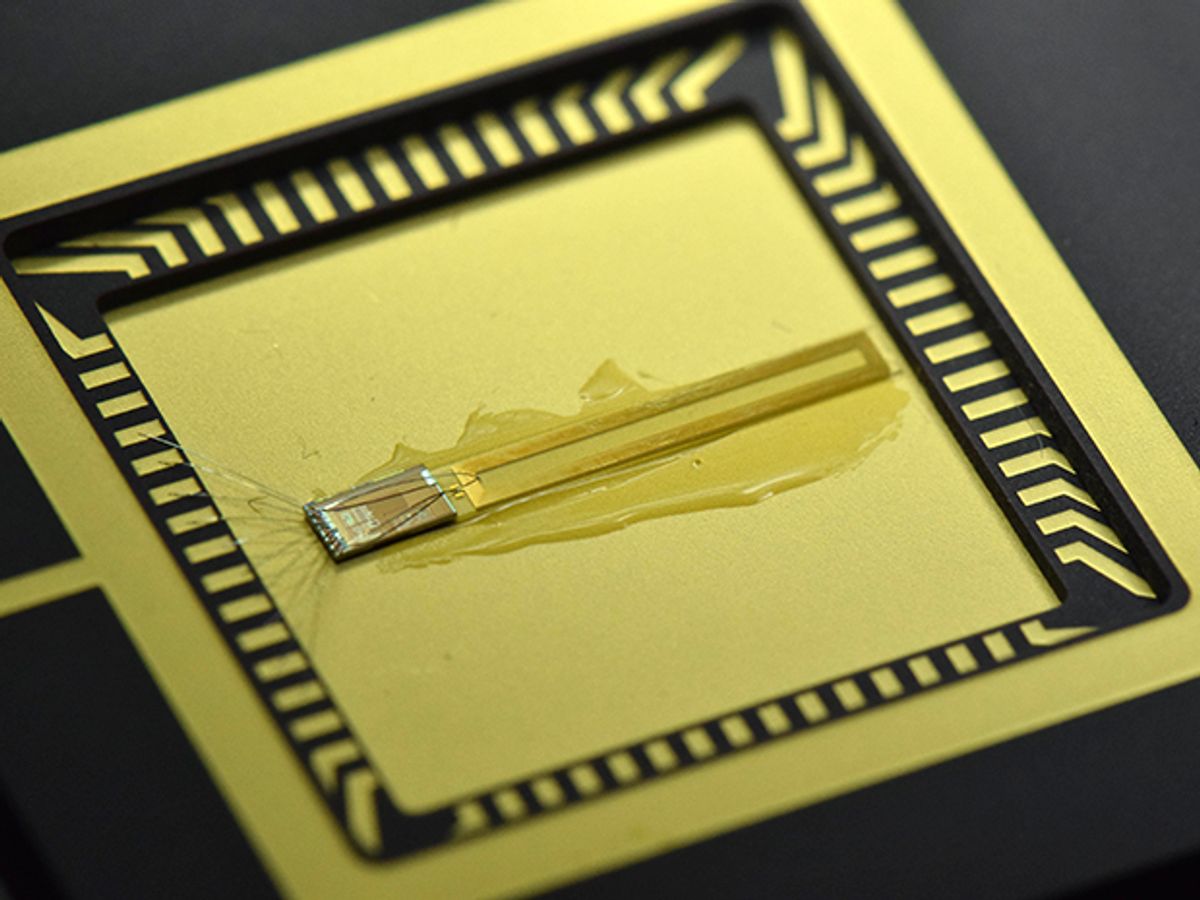
The hardest thing to shrink isn’t the processor. It’s actually the radio, says Blaauw. Last week at the IEEE International Solid-State Circuits Conference in San Francisco, Blaauw and fellow engineers David Wentzloff and Yao Shi showed a prototype injectable radio with a volume of just 10 cubic millimeters (1 mm x 1 mm x 10 mm) that can send powerful radio signals 50 centimeters away, including through 3 centimeters of tissue.
There are two key requirements to get a strong signal from a tiny radio. One is a good antenna design. If you’re making a terrestrial radio antenna you can make it as big as possible to send powerful signals as far as possible. Shi says the Michigan group got around this size problem by co-designing the tiny broadcast antenna with the exterior receiving antenna. They are matched in a way that lets the receiver pick up the weak signal from inside the body. 50 centimeters may not sound that far, says Blaauw. Considering that the antenna in the radio is only 1 millimeter, though, it’s a huge ratio, and certainly far enough to reach a nearby cellphone.
The second requirement is the power source. The standby power of the radio is only about 15 nanowatts, but sending out a signal takes a quick burst of power. The Michigan group had to make their design work with a tiny battery that can’t put out much current at once. So they integrated a capacitor that draws on the battery over time to build up enough energy for a quick burst. “It rapidly dumps that power into the antenna,” says Blaauw. This intermittent transmission means the bits are more spread out than those coming from a usual radio, so the Michigan group had to design a special encoding method. The battery can be recharged by a photovoltaic cell sensitive to the ambient infrared light passing through the body.
Much recent work on implantable or injectable medical devices has centered on using novel materials that are flexible, soft, and squishy. These novel devices can do things like slide through a thin-gauge needle for implantation without the need for risky surgeries, then monitor oxygen, glucose, and other biometrics, or follow disease progression in tumors. In June, for example, researchers at Harvard injected super-flexible nanowire nets into the brains of mice to measure electrical activity. And at CES this January, South San Francisco start-up Perfusa showed injectable hydrogel based oxygen sensors.
Blaauw’s focus is to miniaturize existing computing systems until they are small enough to go through a syringe. There’s no need for such a system to be flexible, the tiny size prevents the rigid system from damaging tissue. The radio is one of many tiny components that the Michigan group has created to be swapped in and out of systems for different applications.
It’s now ready to be integrated with other similarly diminutive components to make an integrated injectable device. The Michigan engineers are collaborating with researchers at the university’s medical school to come up with the first test application. They used the previous, shorter-range version of the radio in a device that sent out information about the pressure inside a tumor. Future devices using the radio may report data from temperature, imaging, pressure, pH, and other measurements.
Katherine Bourzac is a freelance journalist based in San Francisco, Calif. She writes about materials science, nanotechnology, energy, computing, and medicine—and about how all these fields overlap. Bourzac is a contributing editor at Technology Review and a contributor at Chemical & Engineering News; her work can also be found in Nature and Scientific American. She serves on the board of the Northern California chapter of the Society of Professional Journalists.