Brain scientists first discovered how to use light to remotely control genetically-modified brain cells about a decade ago—a breakthrough that has enabled new scientific studies of depression, addiction and Parkinson’s disease. Now a new generation of transparent brain sensors could record brain cell responses without blocking the light’s access to the underlying brain tissue.
The brain control technique that seems to hearken from science fiction, called optogenetics, has traditionally relied on metallic sensors sitting on the surface of the brain to record the organ’s responses to the light stimulation. Some transparent versions of the brain implants have tried electrodes made of indium-tin oxide, a brittle material that is ill-suited to the idea of flexible brain sensors and has limited transparency for certain wavelengths of light. In a study published this week in Nature Communications, a team of U.S. researchers working with a Thai colleague have shown how sensors made from graphene could work much better.
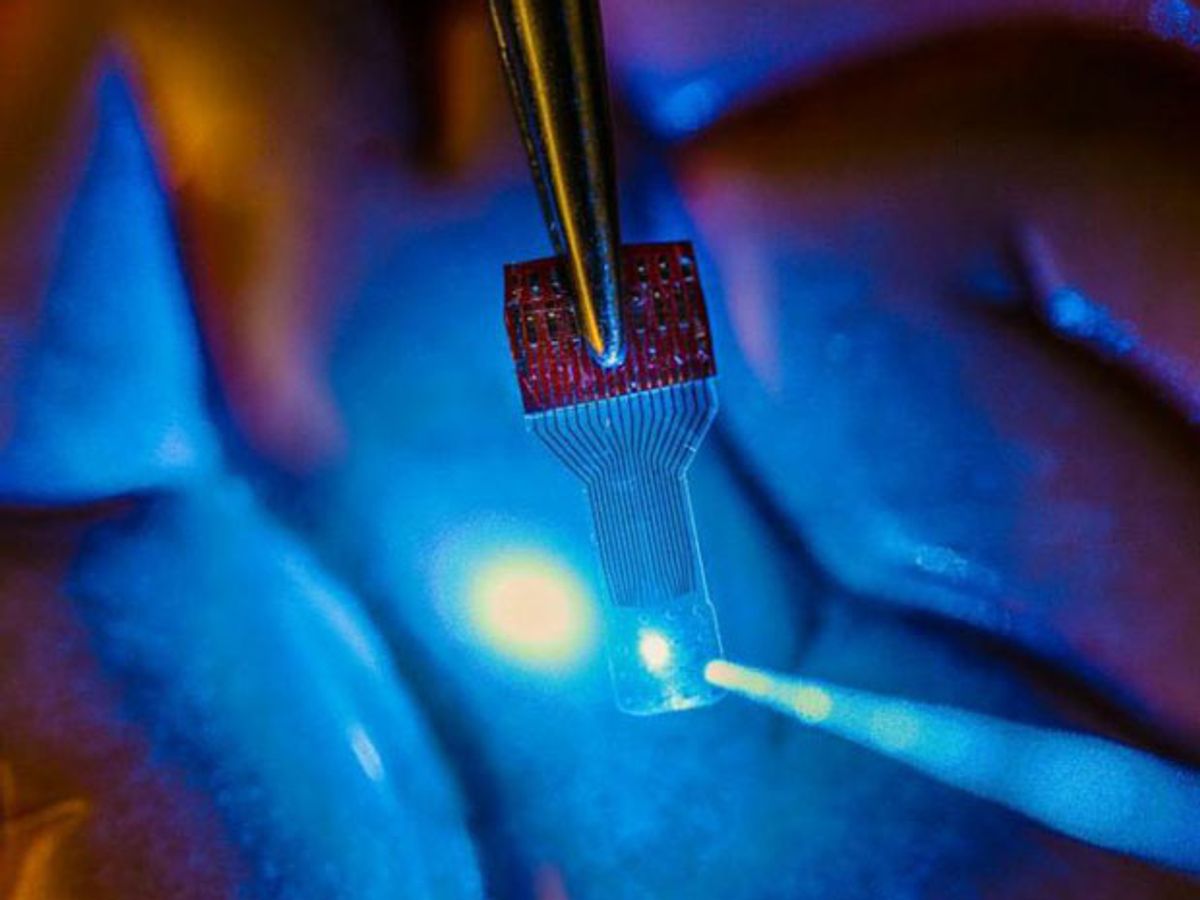
“A traditional implant looks like a square of dots, and you can't see anything under it,” said Justin Williams, a professor of biomedical engineering and neurological surgery at the University of Wisconsin-Madison, in a press release. “We wanted to make a transparent electronic device."
The new device mainly consists of four layers of graphene—each layer just one atom thick—sandwiched between two layers of moisture-proof polymer. Researchers had to strike a balance between having better conductivity with increasing material thickness and having better transparency with a greater thinness. Thinness also helps give the new device its flexibility so that the sensors can adjust to the surface of the brain.
A thin graphene arrangement allowed more than 90 percent of light—from the ultraviolet to infrared—to pass through. By comparison, sensors made from indium-tin oxide allowed 80 percent of light through; traditional sensors made from thin metallic materials allowed just 60 percent . Researchers tested the brain devices by surgically implanting them in lab rats and mice.
“Other implantable microdevices might be transparent at one wavelength, but not at others, or they lose their properties,” said Zhenqiang (Jack) Ma, a professor of electrical and computer engineering at UW-Madison, in the press release. “Our devices are transparent across a large spectrum... We’ve even implanted them and you cannot find them in an MR scan.”
Such transparency should give a boost to optogenetics studies, which have already shown a remarkable ability to control the brain. One of the latest studies looked at using lasers to transform bad memories into good memories in mice.
The new transparent sensors should also be compatible with a wide range of brain imaging techniques that rely on various light wavelengths. That’s crucial for medical researchers trying to understand how new electromagnetic or drug treatments can help patients with brain-related diseases such as epilepsy or Parkinson’s disease.
Transparent sensors could also spawn a wide variety of other medical uses. For instance, the UW-Madison team is working with the University of Illinois-Chicago on putting the transparent sensors on contact lenses as a way of monitoring retinal damage or diagnosing glaucoma early on.
Jeremy Hsu has been working as a science and technology journalist in New York City since 2008. He has written on subjects as diverse as supercomputing and wearable electronics for IEEE Spectrum. When he’s not trying to wrap his head around the latest quantum computing news for Spectrum, he also contributes to a variety of publications such as Scientific American, Discover, Popular Science, and others. He is a graduate of New York University’s Science, Health & Environmental Reporting Program.