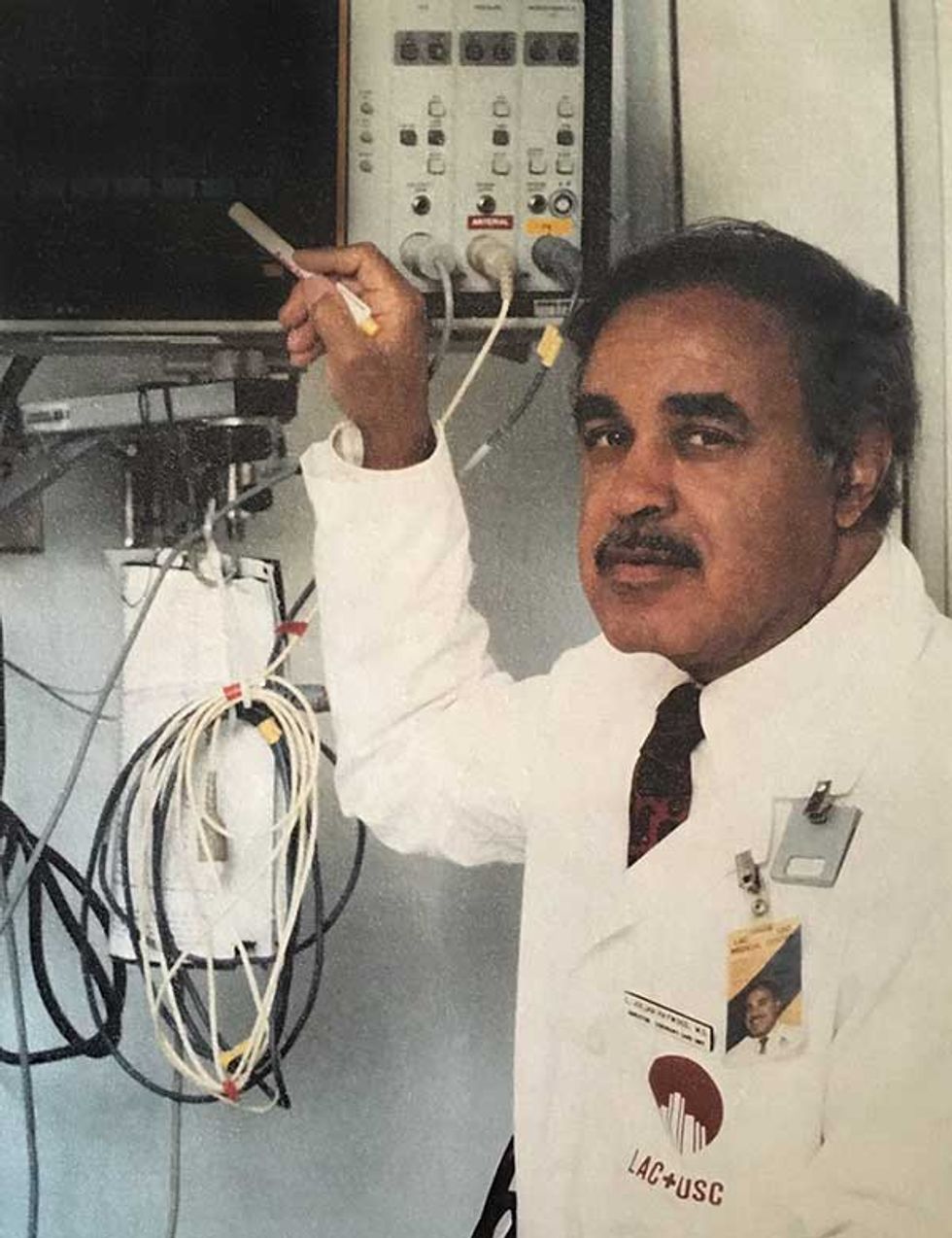
Cardiac arrhythmia—an irregular heartbeat—can develop in an instant and then quickly, and sometimes fatally, spiral out of control. In the 1960s, physician L. Julian Haywood sought a way to continuously monitor the heart for such rhythm changes and alert nurses and doctors when an anomaly was detected. It would be one of many innovations that Haywood and his associates at Los Angeles County General Hospital implemented to improve the quality of care for patients with heart disease.
Haywood had arrived at the hospital in 1956 as an eager second-year resident in internal medicine. Having already completed a residency at the University of Virginia and Howard University, followed by two years as a medical officer in the U.S. Navy, he set his sights on specializing in cardiology.
Haywood was thus deeply disappointed to discover that the hospital had no formal teaching in the area, no clinical cardiology rounds, and no cardiology-related review conferences where doctors and students would gather to discuss patients and interesting developments. This despite the fact that the hospital’s mortality rate among heart attack patients was 35 percent.
Haywood was persistent. He soon learned that Dr. William Paul Thompson presided over a review conference on electrocardiography—the measurement of electricity activity in the heart. These Thursday morning sessions, held in the hospital’s main auditorium, drew faculty from the medical schools at the University of Southern California (USC), the College of Medical Evangelists, and the California College of Osteopathy. The weekly conference set the stage for Haywood’s lifelong investigation into how technology and specialized care could be used to help patients with heart disease.
How heartbeats came to be measured
An electrocardiogram, also known as an ECG or EKG, is a graph of the heart’s electrical activity, measured in millivolts. Today, an ECG is an easy, safe, and painless test that doctors rely on to check for signs of heart disease. In a conventional ECG, a technician places 10 stick-on electrodes on the patient’s chest and limbs. These days you don’t even need to go to a doctor to get such a test: ECG-enabled smartwatches have hit the market that can measure your blood pressure, heart rate, and blood oxygen saturation, all in real time. In the next few years, the same features may be available through your earbuds.
Back in the late 19th century, though, scientists investigating the heart’s electricity activity would puncture the heart muscle with wires. The technology for noninvasively capturing ECGs took decades to develop. British physiologist Augustus Waller is usually credited with recording the first human ECG in 1887, using a device called a capillary electrometer. Invented in the early 1870s by a doctoral student at Heidelberg University named Gabriel Lippmann, the capillary electrometer was able to measure tiny electrical changes when a voltage was applied.
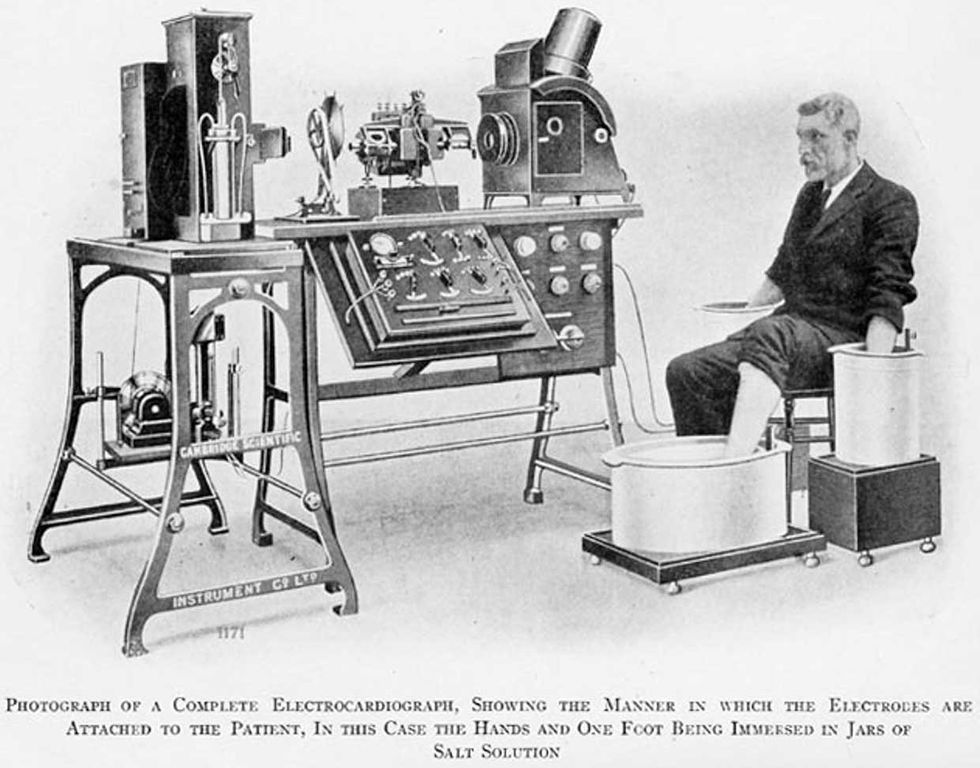
In 1893, Dutch physiologist Willem Einthoven refined the capillary electrometer to show the voltage graph of a heartbeat cycle and the cycle’s five distinct deflections. He named these points P, Q, R, S, and T, a convention that persists to this day. Einthoven went on to develop an even more sensitive string galvanometer, and he won the 1924 Nobel Prize in Physiology or Medicine for his “discovery of the mechanism of the electrocardiogram.” (Einthoven’s string galvanometer was recently approved as an IEEE Milestone, awarded to significant achievements in electrotechnology. For more on the string galvanometer, see “Forget Electrodes, the First EKG Machine Used Buckets of Saline Solution and Telephone Wire.”)
In the early 20th century, ECGs were large, fixed instruments that could weigh up to 600 pounds (272 kilograms). One misconception was that they were overly sensitive to vibration, so early installations tended to be placed in basements on concrete floors. Electrostatic charges could interfere with readings, so ECG machines were often enclosed in Faraday cages.
The first “portable” instrument, introduced in the late 1920s, was a General Electric model that used amplifier tubes instead of a string galvanometer. Although it weighed about 80 pounds (32 kg), it could be loaded on a cart and wheeled into a patient’s room, rather than the patient having to be transported to the equipment. In the 1930s, the Sanborn Co. and Cambridge Instrument Co. came out with the first truly portable ECG systems.
The rise of cardiology as a specialty
Despite this long history of invention, cardiology still did not exist as a specialty when Haywood was completing his residency at L.A. County General. He continued to look for ways to expand his educational opportunities. When he learned that the U.S. Public Health Service provided funding to create special units to care for heart attack patients, Haywood applied, and in 1966 the hospital opened a four-bed coronary care unit. He also secured funding from the Los Angeles chapter of the American Heart Association to start a nurse training program in cardiology.
At the time, the hospital’s standard treatment for acute myocardial infarction (heart attack) included four to six weeks of hospitalization. The goal of the new coronary care unit was to reduce the hospital’s 35 percent mortality rate among heart attack patients.
About 40 percent of those deaths were likely due to arrhythmias, which occurred even when patients were being closely observed. Haywood and his associates knew they needed a reliable way to continuously monitor the heart for rhythm changes. They developed the prototype digital heart monitor shown at top and began using it in the coronary care unit in 1969. The automated system detected heart-rhythm abnormalities and alerted nurses and doctors, either at the bedside or at a central monitoring station. The software for the monitor ran on computers supplied by Control Data Corp. and Raytheon. (Haywood donated the monitor to the Smithsonian National Museum of African American History and Culture in 2017.)
Haywood and his collaborators published widely about their work on the monitor, in Computers and Biomedical Research, Mathematical Biosciences, Journal of the Association of the Advancement of Medical Instrumentation, and elsewhere. Haywood also presented their work at the Association for Computing Machinery’s annual conference in 1972. The monitor influenced the design of commercial products, which were subsequently deployed at hospitals throughout the country and beyond.
The hospital’s coronary care unit and the cardiac-nurse training program were also successful, and mortality rates for cardiac patients declined significantly. Trainees went on to work at hospitals throughout Los Angeles County, and a number of them enjoyed successful careers in education and administration. As other hospitals in the region began creating their own coronary care units, friendly competition resulted in improved care for cardiac patients.
L. Julian Haywood’s legacy of equitable health care for all
Over the course of his distinguished career, Haywood was keenly aware of the disparities in access to health care for racial minorities, as well as the difficulties that minorities faced in gaining acceptance by the medical profession. He was only the third Black internal medicine resident at L.A. County General (now known as Los Angeles County + University of Southern California Medical Center). Nearby, the USC School of Medicine (now the Keck School of Medicine of USC) had yet to graduate any Black medical students (although two were seniors at the time). When Haywood later joined the hospital’s teaching faculty, he was one of the few full-time faculty members who were minorities.
From the time he completed his residency, Haywood was an active member in the Charles R. Drew Medical Society, the Los Angeles affiliate of the National Medical Association. The NMA had formed in 1895 during a time of deep-seated racism and Jim Crow segregation, and its mission was to aid in the professional development of Black physicians, who were for many years excluded from membership and otherwise discriminated against by the American Medical Association.
In the 1960s, a major concern of the Drew Medical Society was the poor access to medical services in the Watts area of Los Angeles. Indeed, the lack of quality health care was one of the systemic injustices that fueled the Watts riots of 1965. In his memoir, Haywood recounts how white physicians tried to bar minority doctors from establishing practices there. Following the riots, the McCone Commission recommended the building of a hospital to serve the needs of South-Central L.A. residents, resulting in the Martin Luther King, Jr. Community Hospital, which opened in 1972.
In 2018, reflecting on his long career, Haywood published an article on the factors leading to a dramatic decline in the death rates for heart disease in Los Angeles County. He concluded that the development of coronary care units in the 1960s helped usher in a new focus on cardiology, leading to progress in angiography (medical imaging of blood vessels and organs), angioplasty (ballooning of arterial obstructions), bypass surgery, and pharmaceuticals to control blood pressure and cholesterol. Additionally, the success of cardiology and cardiothoracic surgery programs at universities spurred research into pacemakers, heart valve replacements, and other lifesaving technologies.
Such progress is impressive and hard won, but we shouldn’t forget: Heart disease is the leading cause of death in the United States as well as the world. The statistics are particularly grim for African Americans, who are more likely to suffer from conditions like high blood pressure, obesity, and diabetes that increase the risk of heart disease. As Haywood noted in his 2018 essay, “The assault on heart disease and high blood pressure continues, as it must.”
Editor’s Note: L. Julian Haywood died of Covid-19 on 24 December 2020. He was 93.
An abridged version of this article appears in the February 2021 print issue as “The Measured Heart.”
Part of acontinuing serieslooking at photographs of historical artifacts that embrace the boundless potential of technology.
Allison Marsh is a professor at the University of South Carolina and codirector of the university's Ann Johnson Institute for Science, Technology & Society. She combines her interests in engineering, history, and museum objects to write the Past Forward column, which tells the story of technology through historical artifacts.



