There are many, many wearable and portable devices aimed at improving life for the blind and visually impaired (in some cases, even restoring vision). Such devices have been developed for pretty much every part of the body: fingers, wrists, abdomen, chest, face, ears, feet, even the tongue.
The thing is—people don’t want to wear them.
“All of these wearables currently on the market have very low acceptance from the community because you look like some sort of RoboCop when you wear them, and people don’t want to attract attention to their impairment,” said Ruxandra Tivadar of the University of Bern in Switzerland, during the annual meeting of the Cognitive Neuroscience Society (CNS), held virtually this week.
Plus, there’s a major unmet need in the field for tools for children, noted Monica Gori, director of the Unit for Visually Impaired People at the Italian Institute of Technology in Genova, Italy. Of the 300 million people worldwide with visual impairments, an estimated 20 million are children, she said. Yet in an analysis of 48 devices available to date, only 2 of them were designed for kids.
During a Tuesday panel at the conference, Tivadar, Gori and other panelists described several new solutions in the field. Here we share a quick glimpse at three of them:

A textured tablet to explore 2D space
We’ve talked about French company Hap2U’s technology before: It’s a haptic interface that relies on ultrasonic vibrations beneath a display surface to create more or less friction against fingertips, producing detailed touch sensations. As a graduate student with Micah Murray at the University of Lausanne in Switzerland, Tivadar (now a member of the cognitive computational neuroscience group at Bern) and colleagues used Hap2U’s technology on a tablet to re-create 2D outlines of an apartment layout. The scientists then asked sighted participants who were blindfolded to explore the textured layout with their fingertips. In this unpublished work presented at CNS, the team found that after exploring a room via touch on the device for 45 minutes (and being trained on sight-less exploration), the participants successfully navigated the real apartment space.
“Digital haptic technology successfully transmits space information,” said Tivadar during the presentation. She and colleagues worked with Hap2U to develop the company’s ability to use textures to represent space. The most practical application, she noted, would be to use the technology directly on a mobile phone in combination with audio and GPS cues to explore a physical space, which Hap2U is already developing.

A sound solution for kids
Over the last decade, Gori’s lab has repeatedly found that blind children often exhibit impairments in spatial sound and touch tasks, such as judging spacing between sounds or identifying the orientation of an object with touch. In the hopes of preventing these perceptual and social delays, “I wanted to have something really simple, a simple sound device that can be processed without any cognitive load or training,” Gori tells IEEE Spectrum. So she created the Audio Bracelet for Blind Interaction (ABBI), a bracelet with an integrated audio system and motion sensors that produces sound to help restore a sense of space in the absence of visual data.
In a study of 44 blind children aged 6-17, the children who used ABBI over a period of three months in a series of training activities improved their auditory and motor skills—and maintained that improvement a year later—as compared to a control group of children who did not use the device.

Restoring sight: Retinal implants and optogenetics
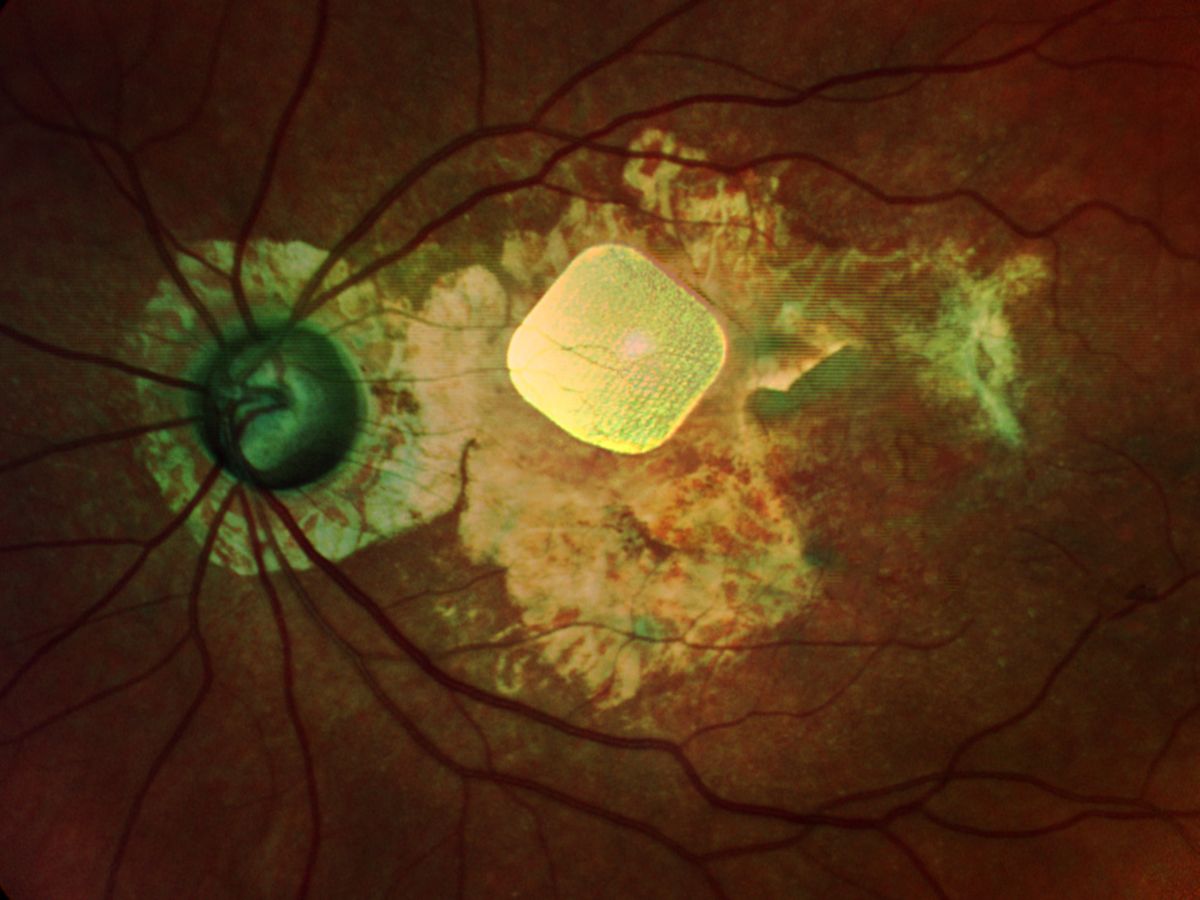
Serge Picaud, director of the Institute of Vision in Paris, France, offered an update on retinal prosthesis and optogenetic therapies—two strategies to restore sight to the blind and visually impaired. After the poor performance of Second Sight’s Argus II implant and closing of Retina Implant AG, he and others are now investigating devices that can stimulate the eye to at least 625 pixels, which should allow some facial recognition. Picaud is working with Pixium Vision in Paris to develop a wireless 378-electrode chip called PRIMA, born out of Daniel Palanker’s lab at Stanford University.
So far, patients with the implant do seem to recover some vision, such as being able to read letters. “Currently patients are reaching a level where they are just below the level of legal blindness,” says Picaud. To achieve 625 pixels, the team could use two implants in one area or slightly smaller electrodes on one implant.

But to achieve the resolution of cells, Picaud’s team has moved into investigating optogenetic therapy, in which a gene is introduced to cells in the back of the eye to make them become photosensitive. Gensight Biologics, of which Picaud is a founder and member of its scientific advisory board, recently moved that work from primates into human clinical trials for patients with retinitis pigmentosa, a rare inherited eye disease.
Megan is an award-winning freelance journalist based in Boston, Massachusetts, specializing in the life sciences and biotechnology. She was previously a health columnist for the Boston Globe and has contributed to Newsweek, Scientific American, and Nature, among others. She is the co-author of a college biology textbook, “Biology Now,” published by W.W. Norton. Megan received an M.S. from the Graduate Program in Science Writing at the Massachusetts Institute of Technology, a B.A. at Boston College, and worked as an educator at the Museum of Science, Boston.