Inside the brain, many neurons fire so that the body will perform a single action like picking up a cup or kicking a ball. Unfortunately for amputees with missing limbs, this brain activity is for naught. Now, engineers at the University of Southampton say they’ve shown that low-power devices known as memristors might be more energy efficient than today’s experimental neural interfaces that help relay signals from the brain to prosthetic limbs.
Themis Prodromakis, who studies nanoelectronics at the University of Southampton, in England, is exploring one of the building blocks of brain and computer interfaces for medical applications. His early research supports the development of special neuronal brain-chips: neural implants that communicate with prosthetic limbs when neurons fire.
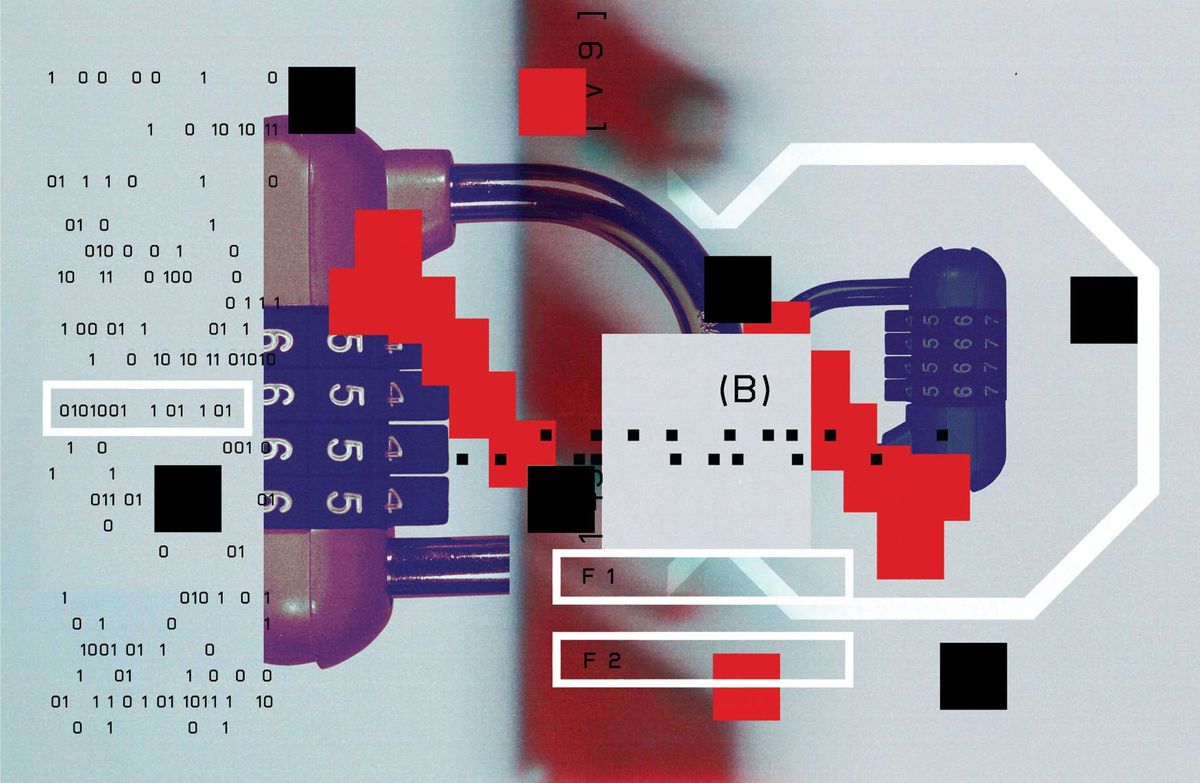
Monitoring thousands of recording sites in the brain and transmitting all that data is a very difficult problem, he says. He told IEEE Spectrum that adding memristors to a system with integrated circuits could allow researchers to monitor activity “from potentially millions of neurons.”
Memristors, the fourth type of basic electronic device—along with resistors, capacitors, and inductors—are special because they have a memory. When current flows, their resistance changes, but the changes remain even after the current is shut off. There’s a scientific movement aimed at using memristors to mimic how the brain learns and processes information.
In the new research, described in a paper published in Nature Communications on 26 September, Prodromakis and his team used memristors for another purpose: recording neuron activity. Recording neuron activity isn’t a new concept; an approach in 2005, for example, used CMOS devices. But it required offline data processing.
In the new experiment, the memristors work in a way reminiscent of the function of the retina in human eyes. Not everything our retina sees gets to the human brain as “it would overload,” Prodomakis says.
Memristors have set voltage thresholds. This lets a memristor, like the human retina, preprocess input signals locally and filter out everything but the important events—in this case, neuron firing activity.
The researchers cultured neurons and hooked them up to an electronic system including memristors. After the system did some preprocessing of the signals, the memristors successfully detected neuron spikes. The memristors then locally compressed the spike amplitude and firing rate.
The ultimate goal, Prodomakis, says, is that the low-power memristors would be hooked up with other devices as an implant to control prosthetic limbs. The next step, he says, is to classify the neuronal activity into different categories.
“This technology is very interesting as a processing tool,” says Max Ortiz Catalan, a biomedical engineer at the Chalmers University of Technology in Göteborg, Sweden. “However, the real clinical application is not very clear or straightforward.”
Ortiz Catalan, who was not involved in the study, works on creating implants for controlling artificial limbs. He notes that the “real bottleneck” in the research field is not processing signals, but finding a way to interface between the brain and prosthetics with long-term stability and high resolution.
“Generally speaking, brain-machine interfaces would benefit from
miniaturization and low-power computational systems,” says Paul Nuyujukian, an engineer at Stanford University who works on brain-computer interfaces for prosthetics. Nuyujukian, who was also not involved in the study, added that, “Work towards that goal is, of course, encouraging to see.”