This article is part of our exclusive IEEE Journal Watch series in partnership with IEEE Xplore.
Hemodialysis is a lifesaving procedure for people with kidney failure, in which a machine can substitute for a patient’s kidneys in filtering their blood, but it involves a lot of clinic visits and laboratory tests. Patients may need to visit a clinic as many as three times a week, and blood samples must be taken before and after each dialysis session to ensure the patient’s blood was filtered adequately. Oftentimes, the process of drawing blood during dialysis causes low blood pressure and dizziness. And without any sort of real-time analysis of how well the dialysis is working, patients must sit through the whole session.
To avoid these repeated blood tests, researchers have developed a new biosensor that provides real-time feedback on the filtering rate as blood is circulated from a patient to the dialysis machine and back. They describe the sensor prototype—and put it to the test—in a study published 20 June in the IEEE Sensors Journal.
Sina Rahmani Charvadeh is a graduate student at the Shahrood University of Technology (SUT), in Iran. In high school, one of Charvadeh’s best friends experienced kidney failure and needed dialysis. His friend told him about the challenges around dialysis and the need for repeated blood tests, which prompted Charvadeh to learn more about the procedure. “[After visiting dialysis clinics] and observing the procedure firsthand, I realized that determining the appropriate time for dialysis in a noninvasive manner can greatly help to reduce the discomforts caused by dialysis and also increase its efficiency,” he says.
Under the supervision of Javad Ghalibafan, an associate professor on SUT’s Faculty of Electrical Engineering, Charvadeh and other researchers set about creating an electromagnetic bandgap structure (EBG) biosensor that analyzes the blood being transferred from the patient to the machine in one tube, as well as the blood returned to the patient in a second tube. As the blood flows through the dialysis tubes, the biosensor uses microwaves to analyze the permittivity of the blood, which indicates the blood’s waste and toxin levels.
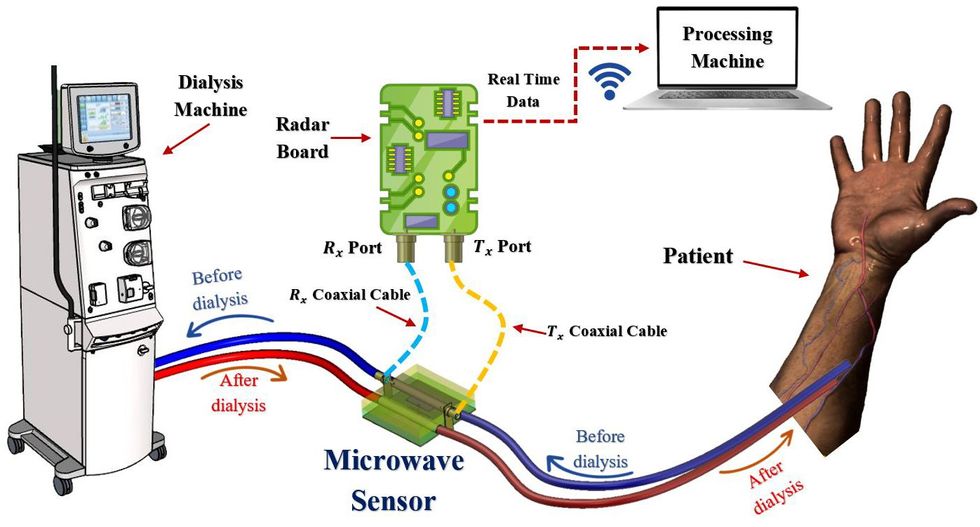
The researchers first used simulations to design the biosensor before creating an actual EBG prototype. The prototype was tested using fake blood, the permittivity of which could be easily manipulated for experimental purposes. The results show that the biosensor can detect relative changes in blood permittivity across samples, suggesting it could provide real-time feedback during dialysis.
Ghalibafan says this biosensor has multiple advantages, including the fact that it is a low-cost, low-power device that does not interfere with the dialysis process—it can be hooked up to the tubes of conventional dialysis machines. Through this approach, patients could enjoy shorter dialysis sessions, if the sensor detects that their blood toxin levels are low enough before the session is scheduled to end.
However, blood can vary from person to person. Ghalibafan says more research is needed to understand how their biosensor works across variable blood attributes. “The next step in this research is to examine more samples, process the measured data, provide measurement patterns, and increase the performance of the proposed method,” he says, noting the team hopes to commercialize the biosensor and provide a practical product in the near future.
This story was updated on 13 July 2023.
Michelle Hampson is a freelance writer based in Halifax. She frequently contributes to Spectrum's Journal Watch coverage, which highlights newsworthy studies published in IEEE journals.