This article is part of our exclusive IEEE Journal Watch series in partnership with IEEE Xplore.
A tiny sensor could one day be placed next to tumors to monitor patients’ responses to cancer in real time. Researchers at the University of California, Berkeley and the University of California, San Francisco, described a prototype sensor in a study published 12 March in IEEE Transactions on Biomedical Circuits and Systems. The researchers used the prototype to demonstrate in a proof-of-concept that the sensor can monitor biological changes in the tissues of mice.
During the early stages of cancer treatment, it can be difficult to assess whether a therapy is working. As of now, the best way to understand how well a patient is responding to therapy is through a biopsy, where small tissue samples of the tumor are taken from patients and analyzed under a microscope in a laboratory. However, biopsies require a lot of time and resources, and ultimately can only provide doctors with a snapshot in time of how well the cancer treatment is working.
“Currently, there is no way to mechanistically monitor response [to treatment] in real-time in tissue deep within the patient,” says Rozhan Rabbani, a graduate student at the University of California, Berkeley. Rabbani adds that implantable biomedical sensors could overcome this issue and provide patients with more personalized treatment plans.
Rabbani and her colleagues set out to create a novel wireless imagesensor in hopes of providing real-time monitoring. The sensor transmits data using ultrasound, which can safely penetrate skin and other bodily tissues. The sensor is also powered by ultrasound, by harvesting the vibrational energy from the ultrasound waves and storing it in an off-chip capacitor.
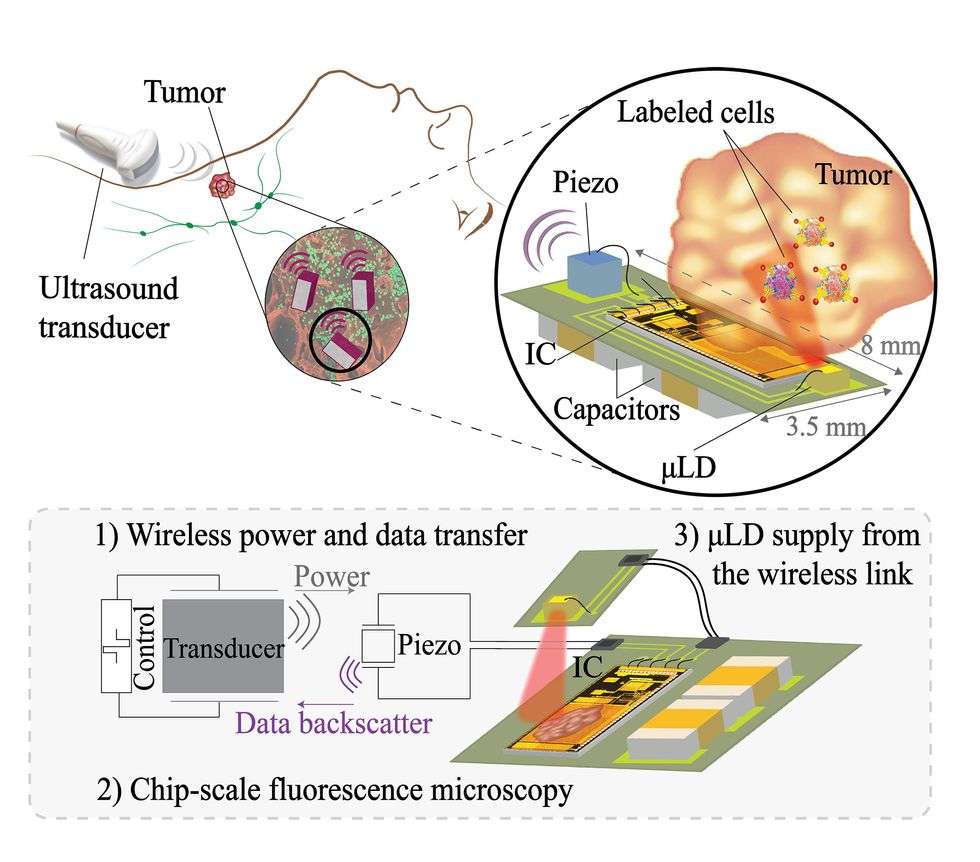
A small laser on the image sensor provides localized illumination, while the sensor itself converts the light into digital signals. Another miniature device, called a collimator, enhances image resolution. “This technology restricts the angle of incident light, resulting in sharper images with higher resolution,” explains Rabbani.
The image sensor, with an integrated circuit just 2.4 by 4.7 millimeters in size, then transmits the data it gathers back outside of a patient’s body, again using ultrasound.
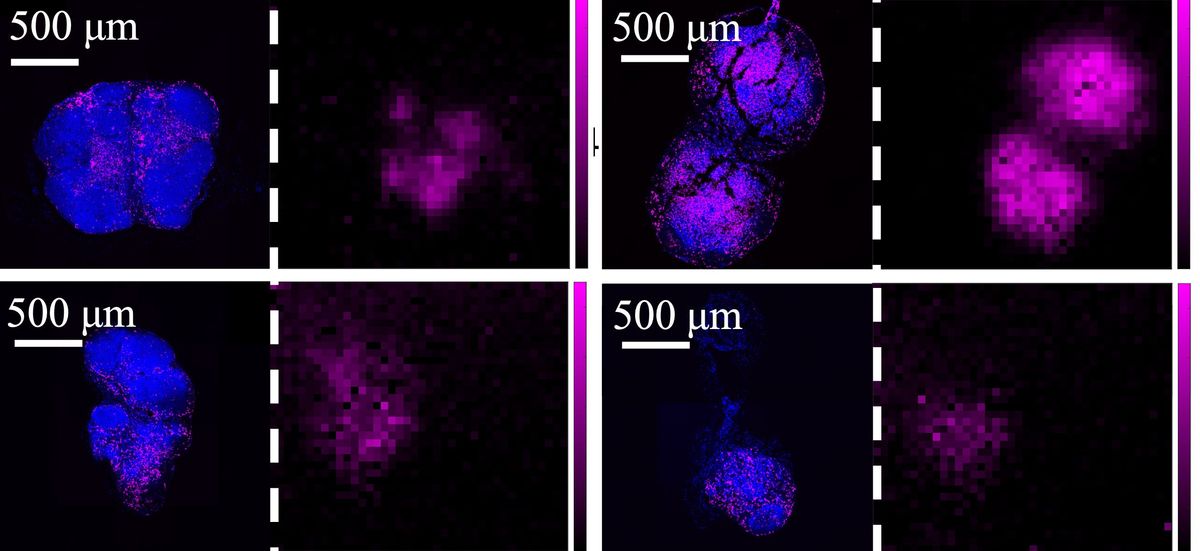
After designing the sensor, Rabbani and her colleagues conducted experiments using mice. For these initial experiments, the researchers did not study tumors in live mice. Instead, they tested the ability of their sensor to simply analyze tissue samples taken from the mice before and after anti-cancer therapy, comparing these images to ones taken by a traditional microscope.
The mice were given anti-cancer therapy, and the tissue samples from the mice were imaged at the beginning of the experiment (untreated group) and after 18 days (treated group). The results show that the novel sensor was able to detect changes in the tissue samples between the two groups as the mice responded to their cancer treatment and more immune cells were found in their tissue samples. For example, the microscope was able to detect a 10 percent increase in the presence of immune cells after treatment, while the image sensor was able to detect a 17 percent increase.
While these results demonstrate that the sensor can capture changes in bodily tissues over time to a similar extent as a fluorescence microscope, more research is needed to ensure the device can safely be implanted in mice and humans without being rejected by the recipient’s immune system.
“Factors such as size, shape, flexibility, and material type play significant roles in determining in vivo biocompatibility,” says Mekhail Anwar, an associate professor at both UC San Francisco’s Department of Radiation Oncology and UC Berkeley’s Department of Electrical Engineering. “Strategies to reduce device size and enhance biocompatibility, such as using organic materials for encapsulation, need to be explored.”
Although the sensor prototype is capable of monitoring clusters of cells over time, its resolution is still not the same as a microscope. Therefore the research team has plans to build upon their sensor’s capabilities. “We are actively working on new technologies to enhance resolution and broaden the application beyond identifying changes in multicell populations,” says Anwar.
“We are hoping that in the future, when we have a fully implantable system, we can monitor the same mouse over time,” Rabbani says.
- Mantis Shrimp Eyes Inspire Cameras to See Cancer ›
- This Rice University Professor Developed Cancer-Detection Technology ›
Michelle Hampson is a freelance writer based in Halifax. She frequently contributes to Spectrum's Journal Watch coverage, which highlights newsworthy studies published in IEEE journals.