Bacterial resistance to antibiotics is a serious threat to public health. It contributed to an estimated 4.95 million deaths in 2019, and a recent review commissioned by the government of the United Kingdom warns that antimicrobial resistance could result in the deaths of 10 million people annually by 2050.
Zapping bacteria with two wavelengths of light—blue LED light and short-wavelength ultraviolet (also called far UV-C)—gives a powerful one-two punch that hampers a known multidrug-resistant strain of E. coli bacteria’s ability to grow and reproduce, scientists in New Zealand have found. In a new study published in the Journal of Applied Microbiology, the scientists report that the dual light treatment could be an effective nonchemical antimicrobial treatment that does not drive bacteria to further increase their antimicrobial resistance.
“The combination of far UV-C and blue-light wavelengths works synergistically to kill the bacteria,” says Gale Brightwell, a principal scientist at AgResearch, a research institute in Palmerston North, New Zealand. “This discovery is exciting, but it warrants further research and verification to fully understand its implications.”
Hospitals have for decades used germicidal UV-C light at a wavelength of 254 nanometers to kill bacteria and sterilize instruments and surfaces. During the COVID-19 pandemic, similar UV-C light-emitting robots and personal sanitizing tools also became important for killing the SARS-CoV-2 virus, which causes COVID. Exposure to this high-energy UV-C radiation for a certain length of time damages the microbes’ DNA or RNA, hampering their normal cellular functions and ability to replicate, eventually rendering them harmless or killing them.
But 254-nm UV-C light can be harmful to a person’s eyes and skin, causing burns, cancer, and cataracts. Researchers have recently shown that far UV-C light, which has a shorter wavelength—222 nm—can safely destroy airborne viruses and bacteria without penetrating human skin or eye cells.
Blue light in the 400- to 470-nm-wavelength range is also known to be lethal to bacterial species that have photoreceptors, which sense the light. The light produces toxic, highly reactive forms of oxygen within the bacteria that damage their cell membranes and the sugary coatings that encase and protect them. It can also mangle their genetic material, which disrupts cellular functions and ultimately impairs their ability to grow and reproduce.
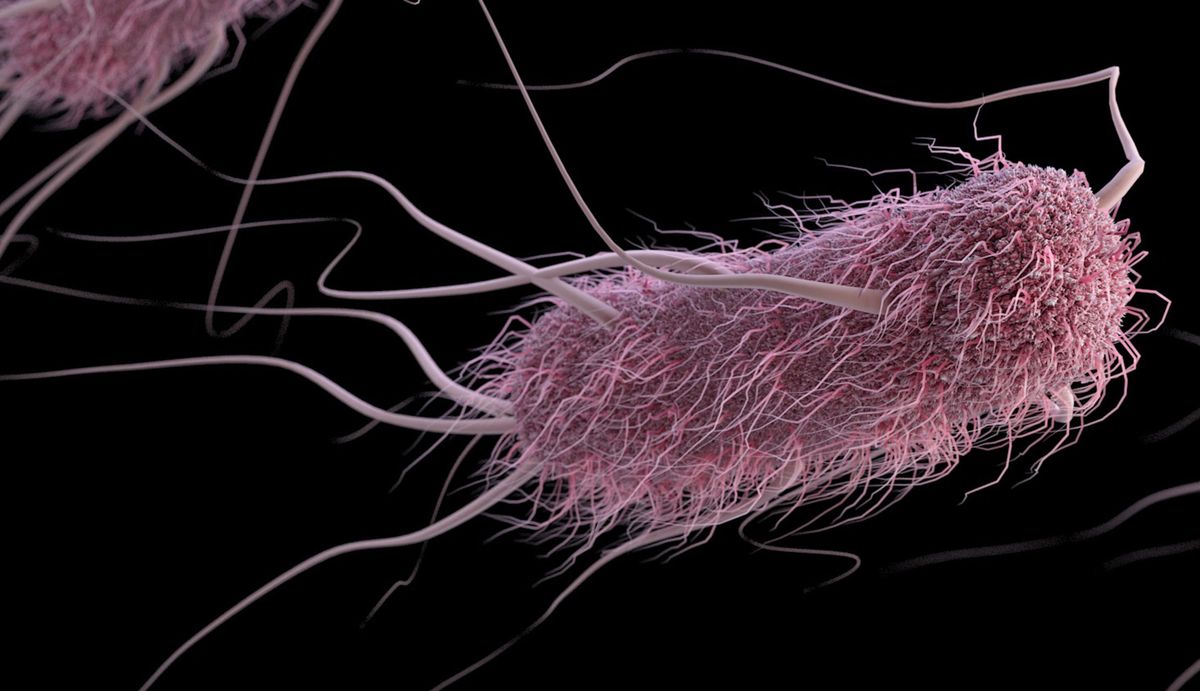
Brightwell and her colleagues decided to see how combining the two types of antimicrobial light would affect a type of bacteria called extended spectrum beta-lactamase E. coli (ESBL E. coli). These bugs produce enzymes that break down and destroy commonly used antibiotics, including penicillin, and “are becoming a significant global threat to human health,” Brightwell says. “They have been linked to higher hospital morbidity and mortality rates, longer hospital stays, and increased health care expenses.”
The team exposed two ESBL E. coli and two antibiotic-sensitive E. coli strains to 222-nm far UV-C and 405-nm blue LED light, both individually and together for a half hour each. They found that the dual light exposure was bactericidal, killing all E. coli strains. Far UV-C light alone did not kill all the bacteria, and individually, blue LED light also showed very little effect on the bugs.
“We believe the blue light inflicts the initial damage to the bacterial cells, making them more vulnerable, and far UV-C then capitalizes on this weakened state to exert its antimicrobial effects more efficiently,” Brightwell says.
The dosage of light was critical. When the researchers exposed all four strains to a sublethal dose of eight long pulses of the dual-wavelength light, the antibiotic-resistant ESBL strains developed light tolerance that was passed onto subsequent generations, suggesting that it may be genetic in nature. The antibiotic-sensitive strains did not develop tolerance. Brightwell says that further research is needed to understand the mechanisms behind this light tolerance and to determine the minimum effective light dose for killing different bacterial strains.
Studies will also be needed to understand how to apply this technology safely, and to help establish regulatory standards and acceptable dosages, given the potential health impact on humans. Far UV-C is generally considered safe, but blue light at 405 nm requires a person to wear safety glasses to protect their eyes. “We believe collaboration with light manufacturers is crucial in ensuring that the technology is safe and effective when applied in real-world scenarios,” Brightwell says.
Nonetheless, compared with standard methods for combating bacterial growth such as chemical or heat disinfection, which consume a lot of energy and water, “using light is a promising alternative, which offers a cheaper, chemical-free, and more sustainable approach to disinfection,” Brightwell says.
- Nanosponges Soak Up Antibiotic-resistant Bacteria and Toxins ›
- Light-Activated Nanoparticles Help Fight Drug-Resistant Superbugs ›
Prachi Patel is a freelance journalist based in Pittsburgh. She writes about energy, biotechnology, materials science, nanotechnology, and computing.