The eight articles that the New York Times published this week in a special Science series on health information technology called “The Digital Doctor” covered everything from advances in imaging technology to the psychological impacts of a wired society. The articles are well worth a read.
One story, on the “ups and downs” of electronic health records (EHRs), examined doctors' and nurses' experiences as EHRs become more wide-spread because of the U.S. government’s multi-billion dollar EHR adoption incentive program. What I found interesting in the Times story was the admission by some of the fiercest advocates for EHRs, like Dr. David Brailer, the first national coordinator for health information technology, that, “The current information tools are still difficult to set up. They are hard to use. They fit only parts of what doctors do, and not the rest.”
Or, as one doctor put it, "Like so many other things in health care, the amount of [EHR] accomplishment is well short of the amount of cheerleading."
Brailer is still a strong advocate who believes EHR benefits far outweigh all the costs and risks involved. He claims that the problems now being experienced will quickly disappear over the next decade as “most of the clunky first-generation tools” will be replaced. Of course, the U.S. government's EHR incentive program will be long over by then, and doctors and especially hospitals, which are spending millions of dollars on their current EHR systems, are going to be stuck with the costs of converting to “Generation-2” EHR systems. My guess is that many hospitals and doctors’ offices won’t upgrade until they absolutely, positively have to do so. Just look at the banking industry and its ever-aging IT systems.
The New York Times article reflects a lot of the debate—and confusion—surrounding the true value of EHRs taking place in the health community. For example, last week the Bipartisan Policy Center released results of a recent survey of some 500 doctors indicating that a “majority of physicians [surveyed] agree that the exchange of health information via electronic health record will improve the quality of care they provide to their patients, especially before and after transitions of care,” says an article at EHR Intelligence. Over 70 percent of doctors in the survey note that the lack of EHR interoperability is a major barrier to patient care. As result of the survey, the Bipartisan Policy Center is calling for the government to increase the incentives to accelerate EHR adoption and their interoperability.
On the other hand, as reported by iHealthBeat, a recently released Physicians Foundation survey of more than 13 000 doctors found that while 33 percent said that their EHR system has improved care quality, 19 percent indicated that they had not, and that they do not anticipate it to do so. Another 13 percent of the doctors survey expect their EHR systems to eventually improved care quality, while yet another 13 percent report that EHRs have had no effect on care quality. Finally, some 10 percent of the doctors surveyed also indicated that their EHR system has decreased care quality and that they do not expect the situation to improve with time.
Of course, in both these surveys, it is impossible to tell what portion of the problems (or benefits) are related to the individual EHR systems themselves as opposed to other factors, such as staff training. I don’t know of any large-scale “apples to apples” comparison of different EHR systems to really understand the benefits, problems, risk or cost issues involved.
Until that happens, expect more dueling EHR surveys, and more arguments over whether EHRs increase or decrease medical costs.
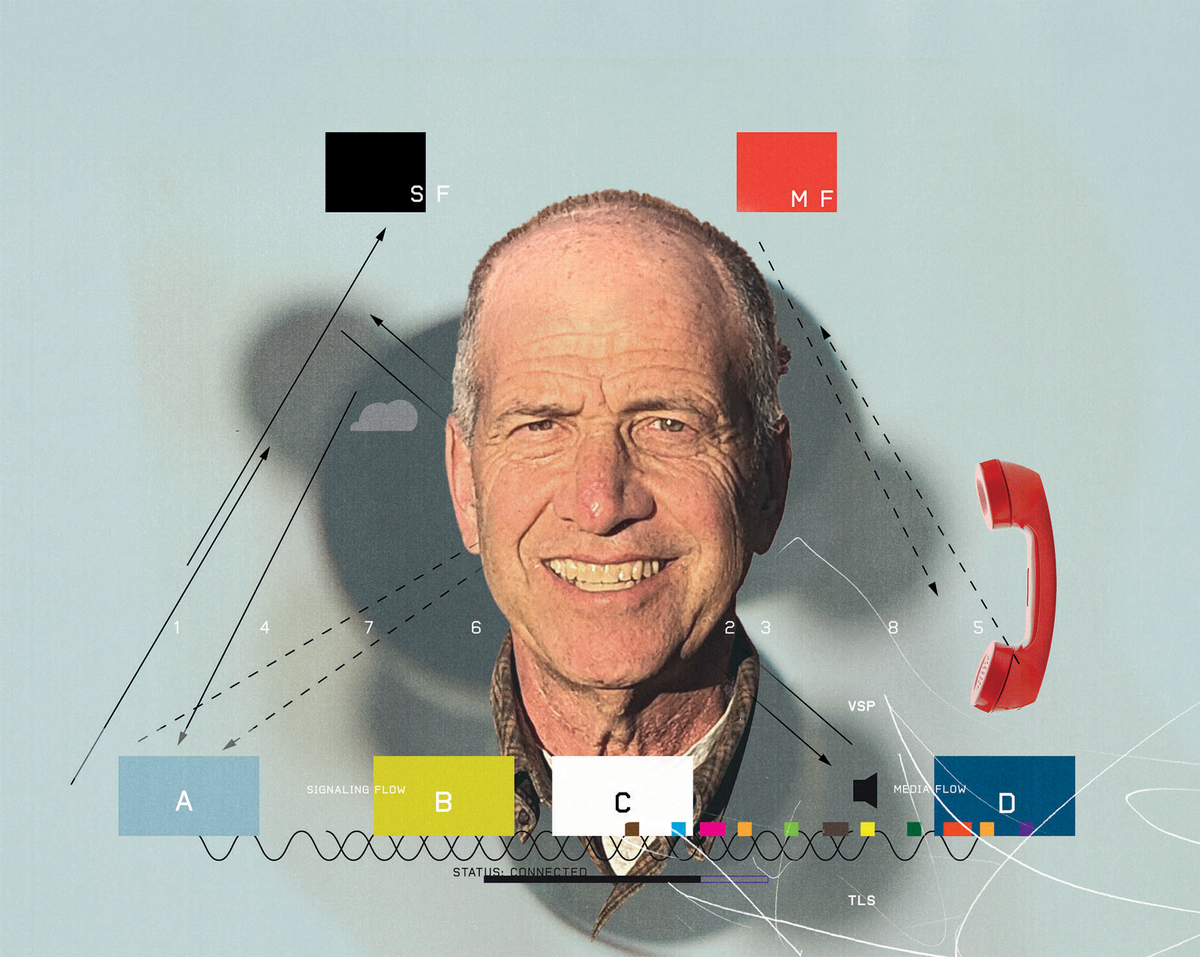
Robert N. Charette is a Contributing Editor to IEEE Spectrum and an acknowledged international authority on information technology and systems risk management. A self-described “risk ecologist,” he is interested in the intersections of business, political, technological, and societal risks. Charette is an award-winning author of multiple books and numerous articles on the subjects of risk management, project and program management, innovation, and entrepreneurship. A Life Senior Member of the IEEE, Charette was a recipient of the IEEE Computer Society’s Golden Core Award in 2008.