A key treatment for heart disease is a procedure known as myocardial resection, wherein a section of diseased or damaged heart tissue is removed. Researchers have been trying to figure out the best way to fill the void where the tissue has been removed. There has been research into creating 3-D scaffolds made from the patient’s own skin cells—structures on which the heart muscle can be regenerated. However, this approach doesn’t provide for a way to continuously monitor and control the development of these tissue patches.
Now, researchers out of Harvard University, led by Charles Lieber, may have found a way to create tissue scaffolds that can be controlled and monitored. The Harvard researchers added this capability by mimicking 3-D nanoelectronic arrays; the results show a way towards real-time mapping and control of electrophysiology in tissues.
In research described in the journal Nature Nanotechnology, Lieber and his team employed a bottom-up approach that started with the fabrication of doped p-type silicon nanowires. Lieber has been spearheading the use of silicon nanowires as a scaffold for growing nerve, heart, and muscle tissue for years now.
In this latest work, Lieber and his team fabricated the nanowires, applied them onto a polymer surface, and arranged them into a field-effect transistor (FET). The researchers avoided an increase in the device’s impedance as its dimensions were reduced by adopting this FET approach as opposed to simply configuring the device as an electrode. Each FET, along with its source-drain interconnects, created a 4-micrometer-by-20-micrometer-by-350-nanometer pad. Each of these pads was, in effect, a single recording device.
“Our latest work shows for the first time a nanoelectronics-enabled scaffold with both size scale and mechanical properties on the same order of magnitude as conventional cardiac tissue scaffold made of FDA-approved biomaterials,” said Lieber in an email interview with IEEE Spectrum. “Compared to previous work, we have reduced the device dimensions by 10x and [made it, mechanically] 1000x softer—which is critical for being matched to the tissue.”
Each tissue scaffold consists of four layers, each of which contains a four-by-four array of the pads described above, along with four circular palladium-platinum microelectrodes that provide electrical stimulation. Sandwiched between each of the four layers are polymer fibers that led to the final scaffold having bending stiffness on par with current technology.
“Our latest work demonstrates an array of more than 100 incorporated sensing devices (64 of which act as monitors), versus only 3 previously,” explained Lieber. “This larger-scale integration of active devices allows for true 3-D mapping of action potentials. Due to the fast response time of nanoelectronics, such 3-D activity mapping has sub-millisecond single-shot time resolution, which greatly exceeds capabilities of optical methods.”
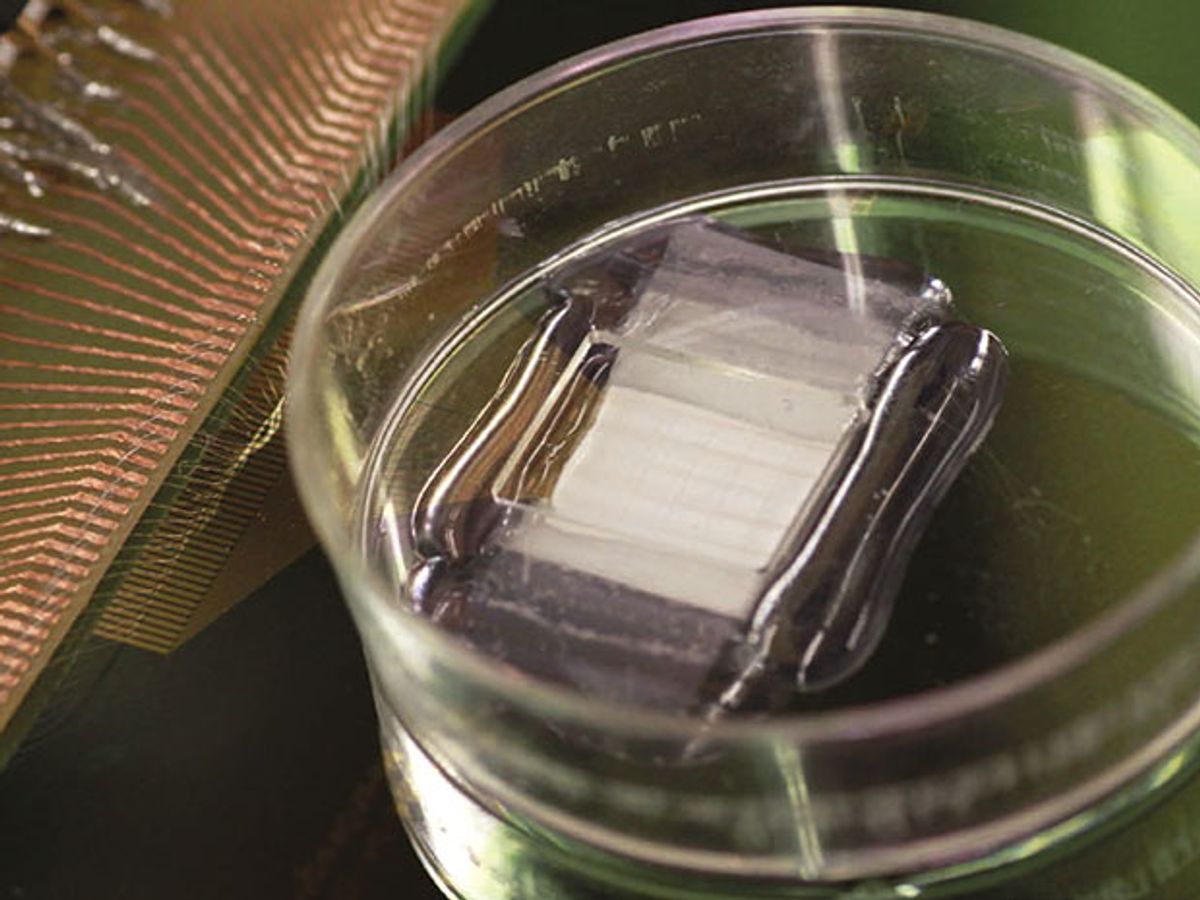
In tests, the researchers put the scaffold into a petri dish containing ventricular cardiomyocyte cells taken from rats. Over the subsequent eight days, the scaffold was able to monitor the electrical activity of the cells.
“Thanks to the 3-D mapping capability, we are now able to use our nanoelectronics-innervated cardiac tissues to study critical problems, including 3-D tissue development, arrhythmia, and drug effectiveness,” said Lieber. “We have also achieved simultaneous mapping and regulation of cardiac activity by incorporating both sensor and stimulating devices, which allows us to ‘smartly’ control the abnormal cardiac activities with continuous feedback from the tissues.”
While the researchers were impressed that the scaffold layout they developed displayed only a 10 percent failure rate in the FET sensors over a two-week period, they concede that the silicon nanowires will eventually fail. In order to overcome this time limitation, the strategy would be to perform a metal passivation of the silicon nanowires in which a light coating of a an oxide is applied as a protective shell that would allow them to provide stable recordings for several months.
This work is best described as proof-of-principal research. However, it does offer huge potential impact in the fields of regenerative medicine and electronic therapeutics.
Lieber added: “The next steps towards implantation would be validation of the capabilities of the smart cardiac patch through implantation in animal models of myocardial infarction.”
Dexter Johnson is a contributing editor at IEEE Spectrum, with a focus on nanotechnology.