A laser-based device has shown it can predict cardiac arrests in rats during open-heart surgery—and it could someday raise the standard of medical care by doing the same for human patients. The amazing predictive quality comes from determining whether or not living cells are receiving enough oxygen to remain healthy and function properly.
No one had previously achieved the tricky task of monitoring oxygen delivery within the living tissue of blood-filled organs, let alone providing predictions about whether a heart might stop beating in the next 10 minutes because the organ’s cells have been starved of oxygen. Lack of oxygen matters because living cells contain mitochondria—the biological equivalent of tiny power plants—that require oxygen to make energy for the cells. Individual cells can suffer damage or death without enough oxygen, which in turn can lead to the failure of living tissue structures such as organs.
“From a medical standpoint, any application in which we want to know whether a tissue is receiving adequate oxygen will benefit from this technology,” says John Kheir, co-director of the Heart Center Translational Research Lab at Boston Children’s Hospital and assistant professor at Harvard Medical School. “[In medicine] we’re often targeting the surrogate measure of a surrogate measure of a surrogate measure, such as blood pressure, when we really want to know whether we’re delivering enough oxygen to living tissue.”
With Kheir providing clinical guidance, his colleagues at a company called Pendar Technologies, LLC successfully developed and tested an instrument capable of assessing oxygen delivery within living heart tissue and predicting cardiac arrest. They also developed software algorithms to filter out background noise and home in on the specific oxygen-related signal they were looking for. But the required breakthrough still required a year and a half of painstaking cooperation between clinicians, scientists, and engineers based in Boston and Philadelphia before achieving the results detailed in the 20 September 2017 issue of the journal Science Translational Medicine.
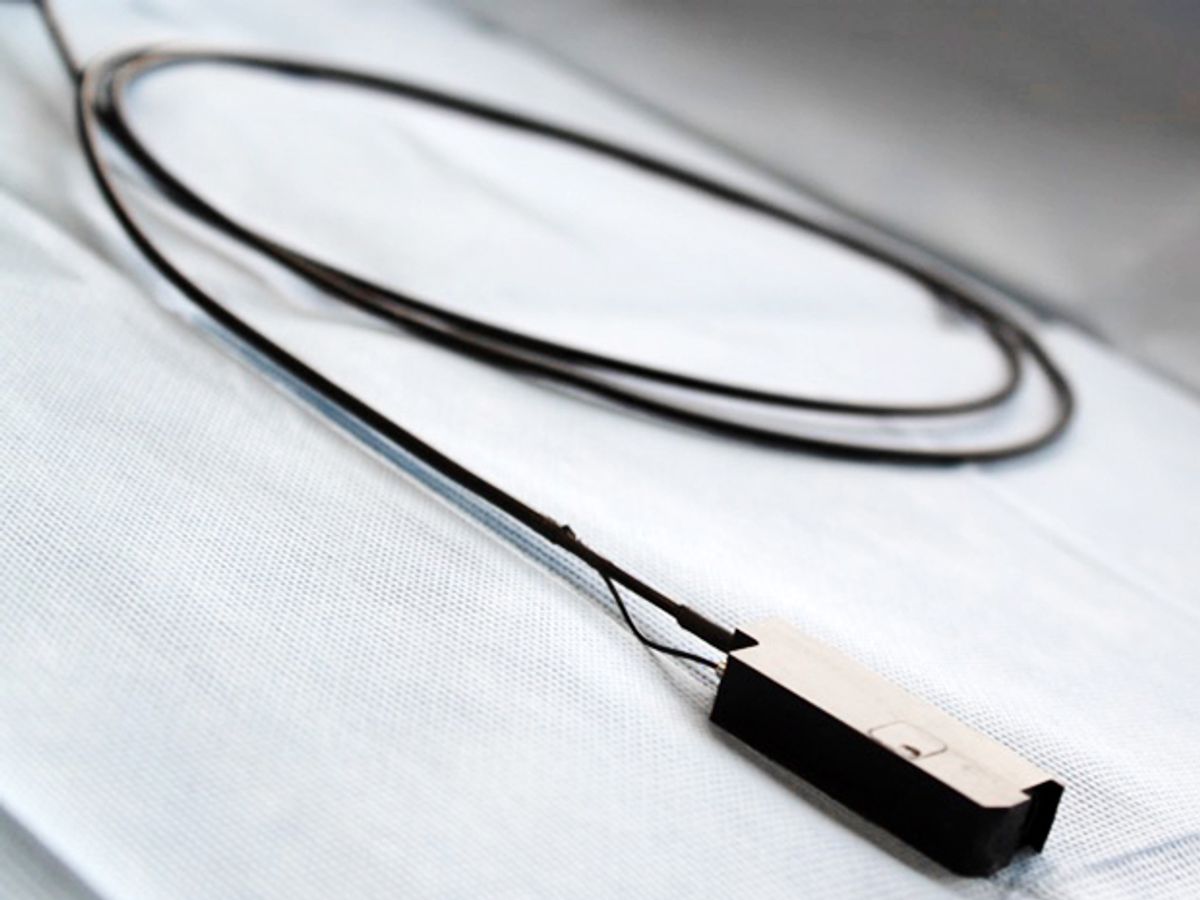
The instrument’s laser probe works by shining a spot of light with the intensity of a laser pointer and the width of a spaghetti noodle directly upon the surface of a heart. The custom-built instrument is based on resonance Raman spectroscopy, a common lab technique that can identify figurative molecular fingerprints based on how light scatters from interactions with the molecules. About 1 in 10 million light photons hitting a given molecule will usually end up dropping to a lower frequency—known as the Raman effect—which can be detected based on changes in the wavelength of the light scattering.

Raman spectroscopy has previously proven capable of detecting whether individual mitochondria isolated in sterile lab conditions are in an oxidized or reduced state. Those two different mitochondrial redox states depend on how much oxygen is available to take up electrons from protein molecules in the mitochondria. Healthy mitochondria function best when they get enough oxygen and have more oxidized molecules as a result.
The researchers decided to focus on revealing the ratio between reduced and oxidized mitochondrial proteins—a measure they describe as the resonance Raman reduced mitochondrial ratio (3RMR). But they faced a major challenge in creating a Raman spectroscopy instrument capable of detecting the 3RMR signal in living tissue such as a beating heart filled with blood. Typically the 3RMR signal would be drowned out by the background noise from the spectral signatures of blood and muscle proteins. Additional background noise can come from the natural light emitted by living tissue that has absorbed some light.
“What John [Kheir] asked us to do was the Holy Grail, which is to measure mitochondrial function in a clinical setting in living tissue as opposed to in a petri dish,” says Daryoosh Vakhshoori, CEO and founder, Pendar Technologies.
The challenge of transforming a lab-based method into a clinical tool was far from trivial, Vakhshoori says. But the researchers succeeded in creating a new and improved resonance Raman spectroscopy platform with 10 times better detection of light signals and reduced the instrument residual error by 10 times. Their hardware can also correct for instrument drift during each spectral scan. Similarly, they fine-tuned their software algorithm to help identify the mitochondrial signature against the background noise of the spectral signatures from blood and muscle proteins.
Next came the testing on rat and pig hearts. A first experiment involved rat hearts removed from the original bodies and perfused with an oxygenated saline solution rather than blood. By precisely reducing the flow of oxygenated saline step by step, the researchers showed that the 3RMR signal would subsequently increase step by step. It was a way of showing that the technology was as good as any other for measuring the 3RMR signal in the absence of messy conditions such as blood.
The second experiment tested the new instrument’s detection capabilities with a beating heart filled with blood during the equivalent of open-heart surgery for rats. Researchers used string to tie off a large vein that normally carries blood from the lower body to the heart, and saw the 3RMR signal increase significantly as blood pressure fell. But they still could not rule out the possibility that the increase in the 3RMR signal came in part from a decrease in interference from the blood protein signal as the heart emptied of blood.
A third rat heart experiment yielded the classic eureka moment and confirmation of all the researchers’ greatest hopes. The researchers lowered the amount of oxygen available while keeping the overall volume of blood the same, so that they could really test the new instrument’s capability to detect a decrease in oxygen delivery to living heart tissue. They were initially so focused on seeing the 3RMR signal change based on the low level of oxygen that they almost missed an exciting realization.

John Kheir had just decided to drop by and observe the ongoing experiments when Dorothy Alison Perry, a researcher at Boston Children’s Hospital and Harvard Medical School, pronounced the data from that animal study “rubbish.” She pointed out that the 3RMR signal had risen, and was confident (based on prior experiments) that the animal was going to suffer a cardiac arrest. In the past, every time the 3RMR signal rose, she said, the animals died before the observation period ended. But Kheir was thrilled by this finding because it showed how the 3RMR signal effectively predicted that the heart would stop beating.
“There is nothing in medicine that can predict cardiac arrest like that,” Kheir says. “We’re really quite excited about that metric as an endpoint in medicine.”
The third rat heart experiment showed that a 3RMR signal of greater than 40 percent was able to predict cardiac arrest with 95 percent sensitivity (correctly identifying when it would occur) and 100 percent specificity (correctly identifying when it would not occur). It also outperformed other laboratory measures that are either too clunky for clinical use or can only make delayed predictions based on leftover biochemical signatures. For now, physicians can only indirectly gauge the oxygen delivery to crucial organs such as the heart by periodically checking the overall levels of oxygen in the bloodstream.
In a fourth experiment, researchers successfully tested the new instrument’s capability to detect the 3RMR signal in the beating hearts of piglets. They chose piglets to make sure that the detection method could work even with thicker heart walls and in larger animals about the size of human babies. That potentially bodes well for eventual human clinical trials.
The biggest next step would involve testing the new instrument’s capabilities in human patients. The current prototype of the new and improved resonance Raman spectroscopy instrument should be up to the task, even with some limitations such as requiring direct access to the surface of the heart (or any organ in question). Another limitation comes from the instrument requiring fairly dark lighting conditions to perform at its best.
The researchers have continuously tinkered with the prototype design, even doing laptop computer modeling in the operating room during experiments, says Padraic Romfh, director of clinical and business development at Pendar Technologies. They were often able to send off orders for a freshly 3D-printed prototype before each day’s experiments finished up. One of the most recent such prototypes involves a probe cover to shield the device from outside light interference.
The ability to predict cardiac arrest could eventually help safeguard patients during operations and during the crucial recovery period that usually lasts for two or three days after surgery. But the new instrument also opens the door to many possibilities beyond predicting cardiac arrest.
Researchers eventually hope to begin studying other organs and surgeries after making a few minor modifications to their device. Such monitoring could potentially help track the state of organs during transplant. Improved monitoring of mitochondrial activities could also help medical researchers better understand the growth and development of such fast-growing cells as cancer cells and stem cells. “This is the first time that we’ve been able to put a number on the adequacy of oxygen delivery,” Kheir says.
Jeremy Hsu has been working as a science and technology journalist in New York City since 2008. He has written on subjects as diverse as supercomputing and wearable electronics for IEEE Spectrum. When he’s not trying to wrap his head around the latest quantum computing news for Spectrum, he also contributes to a variety of publications such as Scientific American, Discover, Popular Science, and others. He is a graduate of New York University’s Science, Health & Environmental Reporting Program.