Surgeons’ best tools for locating tumors inside the body are often their hands. But during minimally invasive surgeries—which can reduce recovery time by days—the ability to examine tissue through touch, called palpation, is lost. Instead, surgeons must manipulate the tissue with long, narrow instruments and rely on visual images from tiny cameras. But engineers in the United States, the United Kingdom, and elsewhere have designed new tools to help restore a surgeon’s sense of touch.
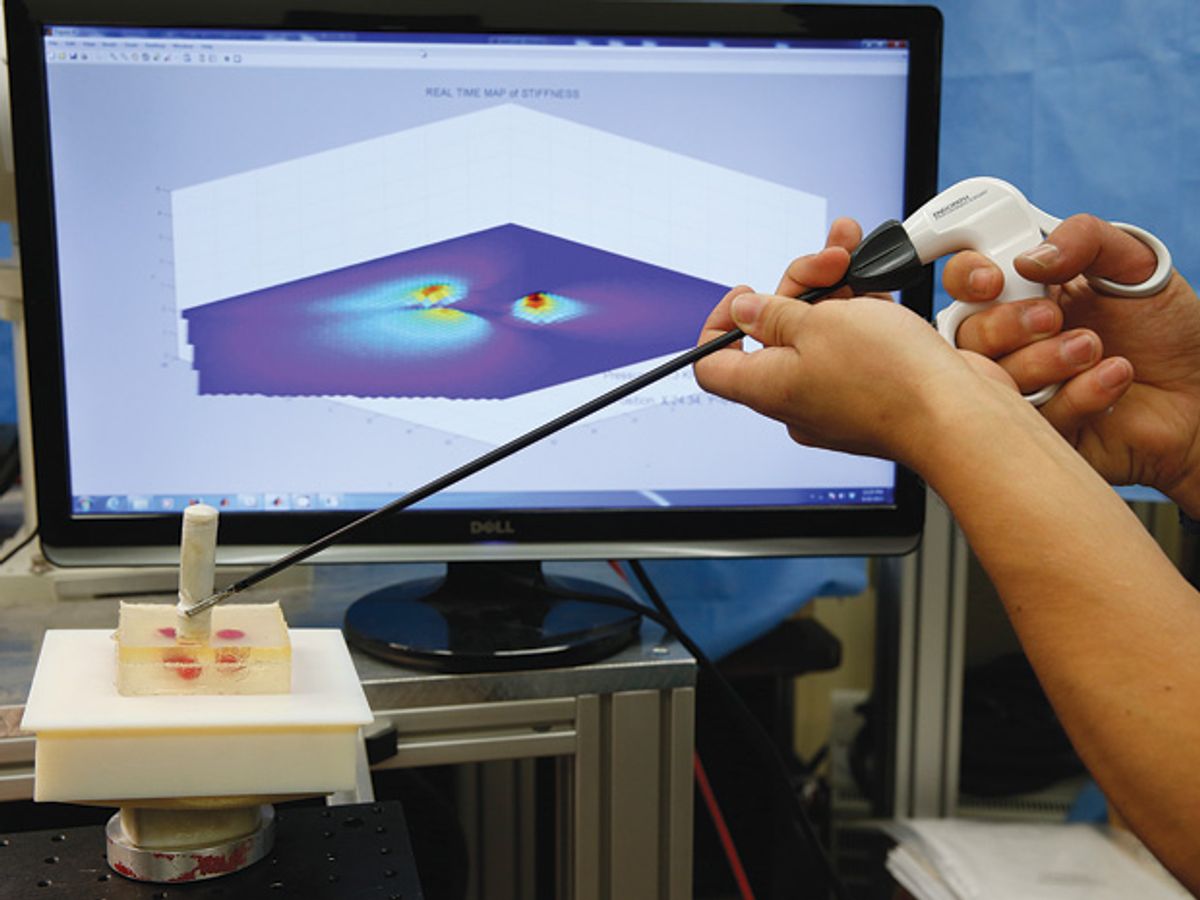
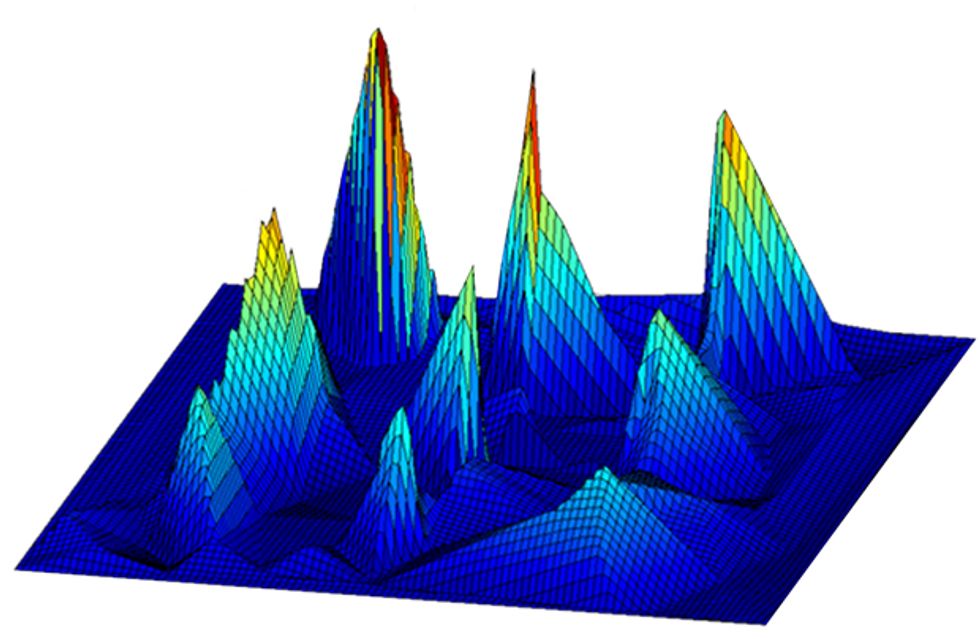
The devices, dubbed palpation probes, are designed to be used laparoscopically and can detect changes in the stiffness of tissue. Tumors are harder than normal tissue, so they can be detected with a combination of pressure sensors and spatial positioning measurements. The readings are used to create a three-dimensional stiffness map that shows surgeons the margins of tumors.
A team at Nashville’s Vanderbilt University led by biomechatronics engineer Pietro Valdastri showed IEEE Spectrum a wireless probe that a surgeon can manipulate in the body with a laparoscopic tool. The small, cylindrical prototype was banged up and wrapped in tape, looking more like something you might find on the floor of your garage than in a surgical suite. But it’s what’s inside that counts—a pressure sensor, a three-axis accelerometer, a three-axis magnetic field sensor, a battery, and a wireless microcontroller.
It works like this: The capsule’s pressure-sensing tip is used to gently indent the tissue. The magnetic field sensor and accelerometer track the depth of the indentation, along with its position relative to a stationary magnet nearby. Each point of contact transmits information about the stiffness of the tissue at that point. Using an algorithm to fill in any unexplored area, the computer creates a 3-D color-coded map that displays the tumors. Valdastri’s team has been testing their probe on a pig’s liver and on a chunk of synthetic tissue that contains tumorlike lumps.
In the pig liver test, Valdastri’s probe was off by just 8 percent in its stiffness measurement. “This new sensor capsule is quite successful in measuring tissue properties,” says Robert Howe, a professor of engineering at Harvard University who developed some of the first remote palpation technologies in the early 1990s.
The novelty of Valdastri’s probe, compared with previous designs, is in its use of a magnetic field sensor to track its position, according to Russell Taylor, director of the Center for Computer-Integrated Surgical Systems and Technology at Johns Hopkins University, in Baltimore. “It’s a very clever way to do it, but it’s certainly not the only way to do it,” he says.
Another group of researchers, this one based at King’s College London and led by robotics expert Kaspar Althoefer, has devised an alternative. Like Valdastri’s prototype, Althoefer’s system tracks the probe’s spatial position, how deeply it indents the tissue, and the reaction force of the tissue. But his design is based on optical fiber technology, and the probe is able to roll over the tissue surface with minimal friction.
Althoefer’s probe consists of three surface-profile sensors equally spaced around a spherical indenter. As the probe glides over a tissue surface, the sphere, which floats on a pocket of air, indents the tissue, and a pair of optical fibers measures the indentation. Another set of optical fibers measures the displacement of the three profile sensors, which move up and down with the tissue surface. The three surface sensors and the spherical indenter work jointly to determine the indentation depth and the force with which the tissue pushes back, making a map of the tissue’s stiffness. The probe has not yet been tested in an animal.
Valdastri’s and Althoefer’s work builds upon nearly two decades of remote palpation research. Previous approaches have focused largely on adding touch sensors to conventional surgical instruments. Many of the technologies have been successfully demonstrated, but none have been commercialized.
The challenge is that the costs of the technologies simply outweigh the benefits to surgeons, say researchers. “If you ask surgeons, they’ll tell you that they need touch feedback, but then they go and perform a vast range of minimally invasive procedures without it,” says Howe. “Touch feedback is in the nice-to-have, not the got-to-have category,” he says.
But Valdastri’s and Althoefer’s probes have some characteristics that might be appealing to surgeons. Because Valdastri’s device is wireless, it is less likely to get in the way of other surgical tools, it doesn’t require a separate incision, and it may allow surgeons to reach places they can’t with a rigid or wired instrument. And because Althoefer’s probe glides over the tissue surface with almost no friction, it is less likely to damage the tissue.
But there are also practical hurdles to address in the quest for perfect palpation. Rajni Patel, a robotics researcher at the University of Western Ontario, in Canada, has developed a pressure sensing array to palpate the delicate tissues of the lung. But one major challenge, he says, has been designing an array that can withstand the surgical sterilization process.
Researchers integrating palpation technologies into surgical robots are also still sorting out how to display the many layers of information to the robot’s operator. That has been a challenge for biomedical engineer Tim Salcudean at the University of British Columbia, in Vancouver. Using a technique dubbed vibro-elastography, he is generating 3-D elasticity maps by exciting tissue with vibration and measuring the waves produced using an ultrasound elastography probe. The probe is held by a surgical robot, which tracks its position. Keeping track of the elasticity map while performing surgery is a lot of work for the surgeon, he says: “How do we display? Is it an overlay or an adjacent image? How do we simplify controls? It is all very challenging, but seeing through the patient is the future of surgery.”
It might not be long before feeling around inside the body during surgery is considered old-fashioned. “The new generation of surgeons are not doing a lot of open surgery, so they’re not used to palpation,” says Salcudean. For those surgeons, computer-generated tissue maps might be all they need to “feel” a tumor.
Emily Waltz is a features editor at Spectrum covering power and energy. Prior to joining the staff in January 2024, Emily spent 18 years as a freelance journalist covering biotechnology, primarily for the Nature research journals and Spectrum. Her work has also appeared in Scientific American, Discover, Outside, and the New York Times. Emily has a master's degree from Columbia University Graduate School of Journalism and an undergraduate degree from Vanderbilt University. With every word she writes, Emily strives to say something true and useful. She posts on Twitter/X @EmWaltz and her portfolio can be found on her website.