Wearable monitors for health and fitness seemed to be everywhere in the exhibit halls and on the conference stages at CES 2016. But while this generation of biometric monitoring devices goes mainstream, a little Silicon Valley company is working on what could be the next generation of body sensing technology: the injectable.
In a small suite high above the CES convention floor, South San Francisco-based Profusa last week demonstrated the Lumee Oxygen Sensing System, the first of what it expects to be a line of biocompatible sensors. This tiny, flexible sensor is about the thickness of a few human hairs and the length of a piece of long-grain rice. It’s made of hydrogel, a substance similar to the material in contact lenses, but is permeated with fluorescent dye. It’s designed to sit under the skin to monitor the levels of oxygen in the surrounding tissue. The company expects to market the device to help people monitor peripheral artery disease, wound healing, and, eventually, for athletes, muscle performance. Profusa has been in stealth mode since 2009, supporting its research with approximately US $10 million in grants and $15 million in venture financing, CEO Ben Hwang told me.
Originally, Profusa planned, Hwang said, to build a better continuous glucose monitor—one that doesn’t trigger a foreign body response that leads to scar tissue buildup—so it can work accurately for years. As a first step, Profusa’s researchers focused on developing the implantable side of the equation rather than the sensing side. They wanted to create an implantable that could be left in the skin forever without triggering the formation of scar tissue or other reactions. They eventually settled on a design that resembles a sponge; it has rounded edges and microscopic holes into which cell tissue grows.
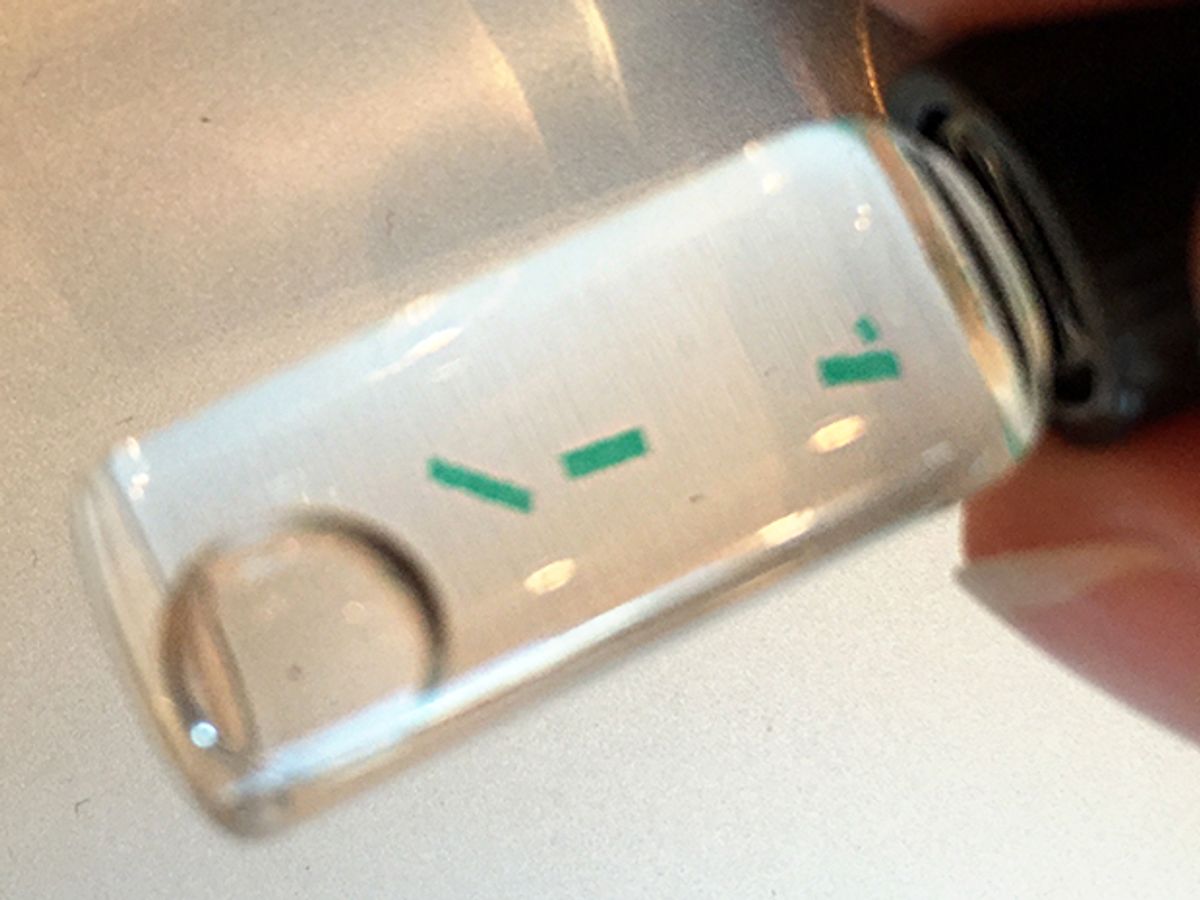
As a test of the prototype, the team embedded the hydrogel sensor with fluorescent dye sensitive to oxygen. The dye glows when excited by particular wavelengths of light; the brightness of the fluorescence diminishes as oxygen binds to chemical receptors in the dye. To read the device, the researchers shine light on the skin above it; an optical reader picks up the emissions. This cycle can happen as quickly as once per second. And while the scanner is currently a handheld device that communicates to a smart phone, Hwang said it could easily be built into a watch or other type of wearable band.
While the oxygen sensing capability was initially planned to be simply a proof of concept (and, perhaps, a method for calibrating other sensors), Hwang said it turned out to have multiple applications of its own. So the company is releasing the oxygen sensor as its first product. Work on the glucose monitor and other sensors—including ones to monitor levels of lactate, creatinine, and urea—continues. Profusa expects its oxygen sensor to receive clearance in Europe for use in monitoring peripheral artery disease within the next few months, with FDA approval on its way. Profusa then expects to seek approval for other applications, including monitoring wound healing and sleep apnea.
To this point, 14 test human test subjects have each had four or so sensors implanted in them for two years; 80 percent of the devices are still working. The company previously conducted tests in rats and pigs. Hwang himself is one of the test volunteers; because you can’t find the sensors by touch, he’s marked his arm to help him quickly find one of them for a demo (though the reader has what Hwang calls a “stud-finder” mode, with colored LEDs that light up to direct you towards a sensor as you scan someone’s body).
Tekla S. Perry is a former IEEE Spectrum editor. Based in Palo Alto, Calif., she's been covering the people, companies, and technology that make Silicon Valley a special place for more than 40 years. An IEEE member, she holds a bachelor's degree in journalism from Michigan State University.