UV Light Might Keep the World Safe From the Coronavirus—and Whatever Comes Next
If researchers can build better UV-C lights, they will be frontline weapons against the next pandemic

Walk into the Cambridge, Ont., office of health-care equipment company PrescientX and you probably wouldn't suspect you're entering one of the most sanitary places in North America.
In this otherwise-ordinary Toronto-area office suite, you can disinfect your keys, phone, and other portables at the reception area's ultraviolet-sterilization stand. In cooler months, the air you breathe is cleansed of mold and bacteria in UV-sterilized heating units as well as blasted by UV fixtures in the office air ducts to eliminate viruses. In-room UV fixtures pointing at the ceiling disinfect the air, while other UV lights that turn on only when no one's in the room zap pathogens on desks, keyboards, and high-touch surfaces in bathrooms and work spaces.
The office, says PrescientX founder and CEO Barry Hunt, represents a possible future in which pandemics like COVID-19 are more commonplace—but in which germicidal ultraviolet light is one of the most potent weapons we have to face them down.
For nearly a century and a half, scientists have been investigating ultraviolet light's deadly effect on germs. In recent times, UV was deployed as a disinfectant against deadly coronavirus particles during the SARS outbreak in 2003. And as soon as the new coronavirus began spreading in earnest in China late last year, UV returned as a potentially powerful weapon to fight this new scourge. While antiviral drugs and vaccines concentrate on minimizing and repelling infections in the body, the ultraviolet systems being deployed focus on killing the virus in the environment, before it has a chance to infect anyone.

Germicidal UV technology is now being used to sterilize air, surfaces, and personal protective equipment like N95 masks. Meanwhile, experts in the field are devoting much of their time to educating the public about the technology's effectiveness against the coronavirus—and outbreaks and pandemics yet to come. The main hurdle for germicidal UV, says Dean Saputa, vice president and cofounder of UV Resources, a Santa Clarita, Calif.–based UV technology company, “is overcoming the lack of...understanding about this technology."
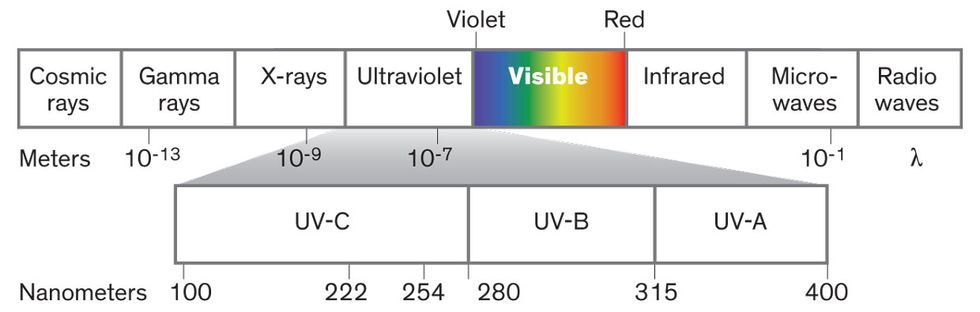
For starters, experts point out, not all ultraviolet rays are created equal. Ultraviolet light lies in a region of the electromagnetic spectrum beyond indigo and violet. Anyone who's read the label on a bottle of sunscreen knows the UV wavelengths that give you a suntan or a sunburn are called UV-A (with wavelengths between 400 and 315 nanometers) and UV-B (315 to 280 nm). Germicidal UV tech focuses on shorter, more energetic UV wavelengths, known as UV-C, which lie between 280 and 100 nm. The Earth's ozone layer prevents virtually all UV-C light from reaching us. So microbes and viruses (and everything else, really) evolved for millions and billions of years without ever being exposed to these wavelengths.
That changed in 1901, with the invention of the mercury-vapor lamp. It produces a potent wavelength of UV-C light—254 nm—that has proved devastating for nearly any genetic material in its path, including that of a coronavirus or a human.
Much of the trick to wielding germicidal UV light against the spread of disease lies in finding a way to keep people safe from that light. Those involved have already built up a lot of expertise in that area, but new technology could make the job of using UV-C in occupied spaces easier.
While UV-C light has been used successfully against germs for more than a century, it's only recently that researchers have understood why it's so successful. In DNA's four-letter alphabet of nucleotides, thymine (T) and cytosine (C) are particularly susceptible to UV. The UV knocks an electron loose and causes two T molecules or two C molecules to bond together, introducing an error into a string of DNA. Humans have genetic self-repair mechanisms, including a molecule called p53. This protein (sometimes referred to as the “guardian of the genome") patrols DNA strands and looks for just this kind of nucleotide damage. But p53 can do only so much. Too much damage overwhelms it and can lead to cancer.
SARS-CoV-2, the virus that causes COVID-19, lacks such sophisticated self-repair mechanisms, and its genetic material is made up of RNA rather than DNA. RNA contains uracil instead of thymine, but the effect of UV-C is essentially the same: Genetic damage accumulates and the virus is destroyed.
The main hitch with UV-C light in the 254-nm range is that it penetrates human skin and eyes, leading to skin cancer and cataracts. So UV-C's DNA-smashing effect means that any disinfecting device that uses it has to be designed to operate either when no one is in the room or in a self-contained space where humans can't go.
Researchers have been trying to balance the benefits and dangers of UV-C for decades. In the late 1930s and early 1940s, the U.S. epidemiologist William F. Wells installed UV-C–emitting mercury-vapor lamps in Philadelphia schools to combat an outbreak of measles, as a follow-up to his groundbreaking work that showed airborne bacteria and viruses could cause infection. The fixtures were designed to irradiate the air only in the upper portion of the room, to protect students and staff from exposure to the rays. And they worked. Schools that had the air-sanitizing equipment experienced a 13.3 percent infection rate compared with 53.6 percent for the population at large.
Germicidal UV in most commercial and industrial settings today still comes from mercury-vapor lamps, says PrescientX's Hunt. These devices have a spectral peak at 254 nm. That emission is the result of an arc of electricity that ionizes (typically) argon gas and vaporizes liquid mercury. Glass would block the radiation, so these lamps are made of quartz instead.
UV-C–emitting LEDs, made from alloys of aluminum nitride, are much newer and have a number of potential advantages over mercury lamps—no toxic mercury, greater durability, faster startup, and emission at a diversity of wavelengths, which may aid in their germicidal role. Most important, though, is UV-C LEDs' theoretical potential for higher efficiency. That potential is as yet unrealized, however. Jae-hak Jeong, technical research fellow and vice president at Seoul Semiconductor, told IEEE Spectrum that today's mercury lamps have a higher wall-plug efficiency—electrical power in versus optical power out—than the UV-C LEDs on the market now. But mercury lamps' advantage is not expected to last, because researchers predict UV-C LEDs to improve in much the same way that blue LEDs did to reach their dominant position in lighting. For now though, UV-C LEDs aren't powerful enough to sterilize more than small volumes of air or nearby surfaces.
Recent experience with UV-C light confirms what Wells found in the 1930s: Air disinfection with 254-nm UV light is “very effective," Hunt says. Direct illumination of the air in the upper part of a room produces better throughput than irradiating the air inside HVAC units, he adds. According to the Illuminating Engineering Society, 17 milliwatts of 254-nm-lamp radiation per cubic meter of upper-air space is the evidence-based dose developed to control tuberculosis. However, some bacteria, viruses, and other microorganisms are more resistant to UV-C light than others.

At that dose, upper-air fixtures can destroy germs in the lamps' direct line of sight “in a matter of seconds," says Saputa of UV Resources. To keep humans safe, the fixtures, which typically cost a few thousand dollars each, are placed at heights above 2 meters, and nonreflective baffles direct the ultraviolet energy upward and outward. (UV-C reflects poorly off of most surfaces, so there's little danger of exposure from rays bouncing off ceilings and other fixtures; nonetheless, installers must make sure by using UV-C meters.) Such installations can be used in a variety of settings, including patient rooms, waiting rooms, lobbies, stairwells, and emergency-room entrances and corridors.
Air isn't the only thing that needs disinfecting. During the pandemic, UV-wielding robots in hospitals and UV germ zappers in airplanes and subway cars have joined a host of technologies being rolled out to disinfect surfaces.
The main difference between these systems and UV air sterilizers is that the former can't operate when people are present, so they're not continuously keeping areas virus-free. “Design engineers must keep in mind disinfection only lasts until people are placed into that hospital bed or sit in that airplane seat," says Saputa.
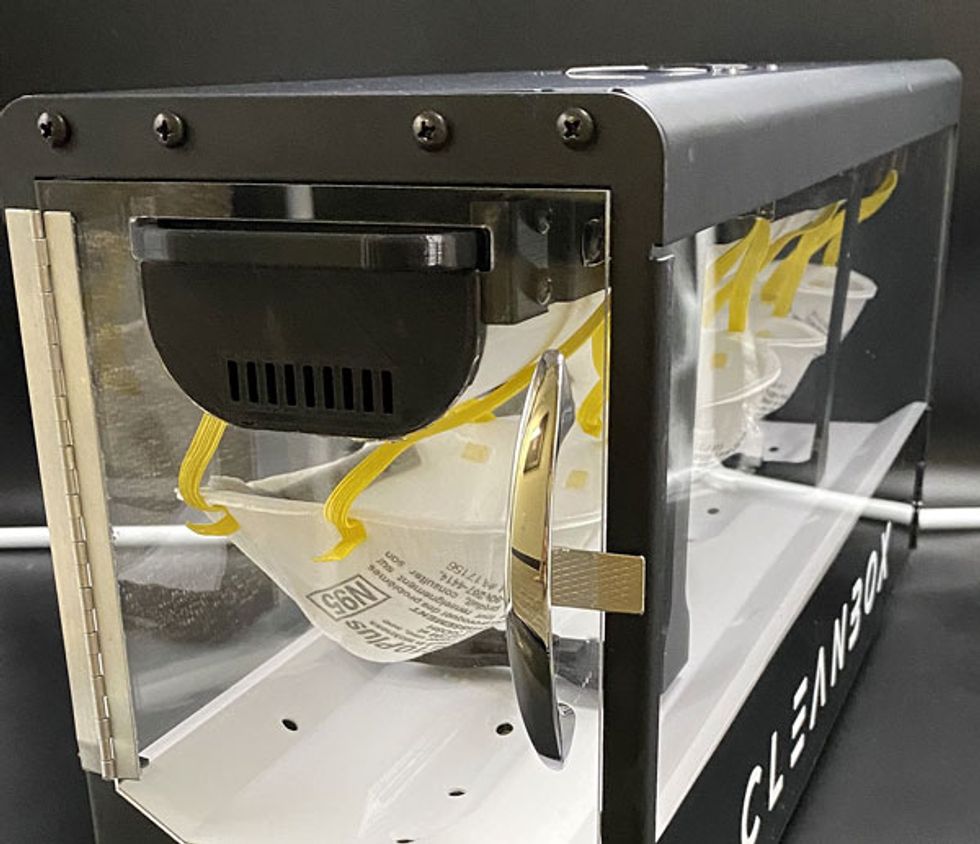
But sporadic disinfection is preferable to none at all. Before this year, Carlsbad, Calif.–based Cleanbox Technology had been developing a UV-C LED box to sterilize virtual-reality and augmented-reality headsets. The company's system was readily adaptable to sterilizing N95 masks, says Cleanbox's chief technology officer and cofounder David Georgeson.
The result, the CleanDefense N95 sanitizing light box, can hold four masks at a time. The box is portable and powered from the wall or a battery bank, enabling use in mobile environments like ambulances and airplanes as well as in health care settings, restaurants, and shopping centers.
The challenge with this technology and any other type of UV disinfection is that “the radiation has to actually strike the virus to break the [RNA] and inactivate it," says Robert Karlicek, director of Rensselaer Polytechnic Institute's Center for Lighting Enabled Systems & Applications, in Troy, N.Y. “If those virus particles are sitting behind dirt or covered by another fiber, you'd have to scatter a lot of light before you got a good kill rate."
The problem is illustrated by what's called the “canyon wall" effect. To bacteria and viruses, textural features on common surfaces can be like 100-meter-deep canyons would be to us. In experiments with surfaces having submillimeter texture, UV-C's kill rate against the bacteria Staphylococcus aureus varied as much as 500-fold depending on the angle at which the mercury lamp's light fell.
That dependence on angle is why it typically takes three UV systems to disinfect a hospital room, according to Marc Verhougstraete, assistant professor of public health at the University of Arizona. Even then, there are still unexposed areas. So for that application, UV-C surface sanitizers should be part of a system that includes routine surface disinfection, hand hygiene, and air treatment, he says.
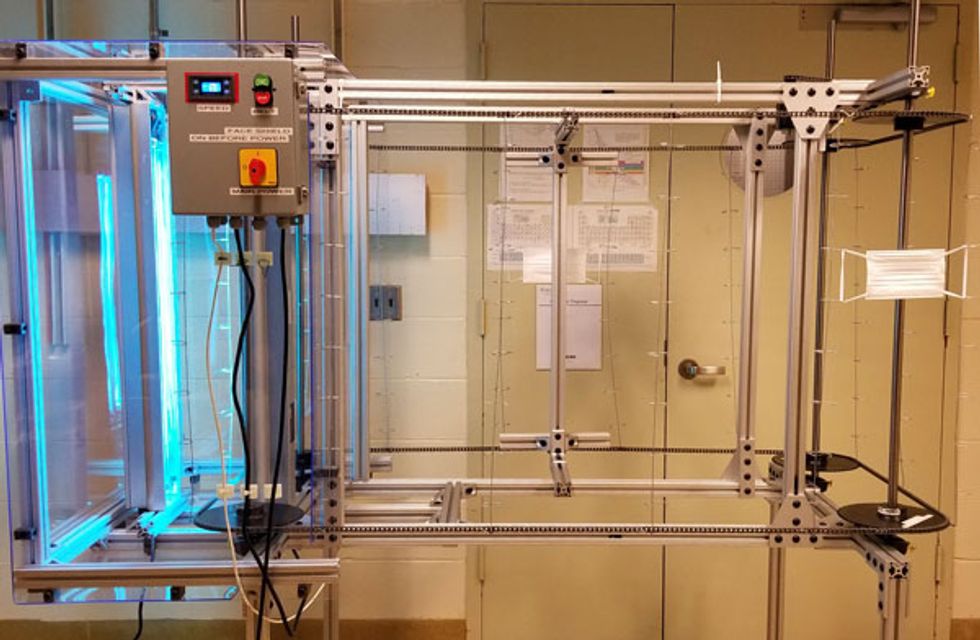
Getting a thorough dosage from more than one angle is key to sanitizing N95 masks for reuse. Karlicek and his team developed a mercury-lamp N95-mask sterilizer that was tested at Mount Sinai Hospital in New York City. It uses two sets of UV lamps to irradiate the front and back of the masks at the same time. PrescientX is also getting into the N95-mask-sterilization business with a UV-C light box called Terminator CoV. And there are other systems in various states of development and commercialization as well.
The precise UV-C dose needed to inactivate a SARS-CoV-2 virus particle is yet to be determined, says PrescientX CEO Hunt. But, he adds, a number of peer-reviewed studies have looked at UV-C doses for the H5N1 and H1N1 strains of influenza and for previous coronavirus outbreaks, including MERS and SARS. Experts think it's reasonable to assume that a similar amount of energy will inactivate the coronavirus that causes COVID-19.
Those studies all found that irradiating masks with 1 to 2 joules of UV-C energy per square centimeter was sufficient to inactivate between 99.9 and 99.99 percent of the virus particles on the mask. That said, eliminating coronavirus particles is not just a numbers game. If the sterilization unit casts any shadows on the mask, that mask will not be fully disinfected. That's why these systems are designed with fasteners and hooks that stretch the mask and minimize shadows.
“You need intensity and geometry to get rid of the virus," Hunt says.
Given the harmful effects of 254-nm UV-C, scientists are exploring the higher-energy wavelength of 222 nm, in the far-UV region. This wavelength has been found to kill viruses and bacteria, and initial studies show that it's substantially safer than photons in the 254-nm range. In fact, far-UV may be able to safely bathe an entire room in sterilizing light, even with people present.
Far-UV light at 222 nm “hardly penetrates the outer layer of skin," says David Sliney, retired manager of the U.S. Army's Laser and Optical Radiation Program at the Army Public Health Center, near Baltimore. “It's heavily absorbed by protein. But there is some evidence that it may even be more effective against airborne viruses" than other UV light. The wavelength appears to be safe for the eyes as well because it penetrates no deeper than the layer of tears that coat the eye. A 2019 study of albino rats in Japan found prolonged far-UV exposure induced no skin or eye damage.
At present, far-UV is generated by krypton-chlorine excimer lamps. (“Excimer" is a portmanteau of “excited" and “dimer," meaning an excited state of a two-part molecule.) Inside the sealed quartz-glass chamber of such a lamp, krypton and chlorine are heated by electric discharge whose energy is sufficient to momentarily create a KrCl excimer, which spits out a 222-nm spectral line before dissociating again.
However, these light sources don't just give off far-UV light. “Excimer lamps produce a peak at 222 nm, but they also produce [longer]-wavelength light," explains David Brenner, director of Columbia University's Center for Radiological Research, in New York City. “And that is damaging, because it doesn't have the protective properties of 222 nm. It can penetrate [skin] and damage DNA."
Filters can eliminate the extraneous wavelengths, but Brenner says a better solution would be a far-UV LED lamp with a narrow spectral profile right at 222 nm. Such an LED does not yet exist. “LEDs have been coming down in wavelength for a long time," he says. “Once you go down below 250, 240, 230 [nm], the efficiency falls off dramatically. It's like a cliff."
So in the near term, excimer lamps are the best hope. Brenner expects such lamps to be on the market by the end of this year or early 2021.
Despite this arsenal of ultraviolet technologies—UV-C LEDs, mercury vapor lamps, and KrCl excimer lamps—the current pandemic may yet come and go before the world has rolled out germicidal UV broadly enough to make a big impact. And so experts are already planning for the next dangerous pathogen, and when it comes, they hope to greet it with a phalanx of UV air purifiers and surface sterilizers in hospitals, airports, public transit, offices, schools, nursing homes, stores, restaurants, elevators, and elsewhere. The ubiquity of UV technology should make it much harder for an outbreak to spread, perhaps preventing a lethal contagion from ever becoming a pandemic.
This article appears in the October 2020 print issue as “The Ultra-Violet Offense."