Treating mental illness doesn't always refer to talk and prescriptions. Psychiatrists nowadays are increasingly embracing innovative technologies that alter neural circuits electrically instead of chemically. Still, the growing field of "brain stimulation" treatment has been consistently stunted by one big uncertain question: what regions of the brain should you target to best help the patient?
New research from Beth Israel Deaconess Medical Center (BIDMC) in Boston could finally provide some clarity. The findings, reported in the Proceedings of the National Academy of Sciences (PNAS) paint a map of “functionally-connected” sites in the brain that better illustrate which brain networks are affected by different diseases—and how psychiatrists can best go about treating them through brain stimulation. They may one day reveal sites in the brain where noninvasive forms of stimulation—like transcranial magnetic stimulation—could be administered in lieu of invasive ones—like deep brain stimulation implants—and still be just as effective.
“Although different types of brain stimulation are currently applied in different locations, we found that the targets used to treat the same disease are nodes in the same connected brain network,” says BIDMC's Michael Fox, one of the study’s researchers. He hopes the results will help psychiatrists make more informed decisions when evaluating treatment options.
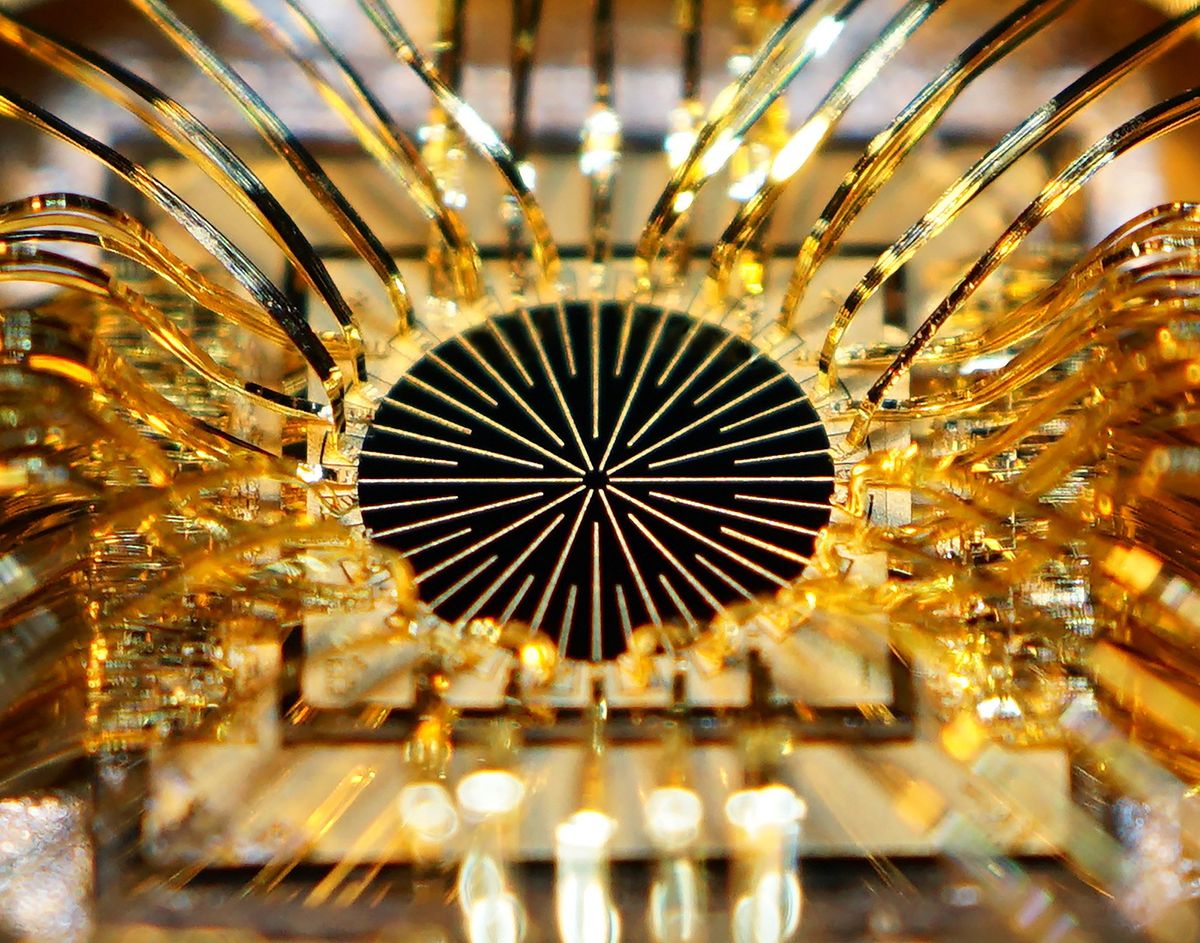
The most widely used brain stimulation—deep brain stimulation (DBS)—requires an electrode to be implanted deep within the brain. Neurons in the area are stimulated at at least 100 Hz. In the last decade, DBS has been a successful treatment option for patients with Parkinson’s, dystonia, and essential tremor.
Repetitive transcranial magnetic stimulation (rTMS) on the other hand, is a noninvasive approach that uses a powerful electromagnet placed on the scalp to stimulate brain cells up to several centimeters below the surface. It provides less frequent and less powerful stimulation, and does not carry the same risks that invasive surgery does. However, the FDA currently approves rTMS for the treatment of depression only.
With some exceptions (such as treating Parkinson's with DBS), there is a lack of information about which specific brain regions should be targeted when treating diseases with brain stimulation; this is especially true for noninvasive interventions like rTMS. When using rTMS to treat depression, there is little agreement on which regions to stimulate to alleviate symptoms. “We don’t know exactly where to go,” says Fox. “This might help to verify where best to stimulate for patients.”
For the study, Fox and his research team looked at brain stimulation treatment data for 14 conditions, including addiction, Alzheimer’s, depression, dystonia, epilepsy, essential tremor, Huntington’s, and Parkinson’s. They listed the stimulation sites, deep in the brain and near the surface, thought to be effective for the treatment of each disease. Fox and his team wanted to determine if some of these sites were actually connected to one-another as part of the same brain networks—and if so, where they were located.
Through a data set of functional MRI images of people’s brains at rest, the research team found fluctuations in spontaneous brain activity that correlated with one-another, illustrating which sites were functionally connected. The researchers drew a map of connections from deep brain stimulation sites to the surface of the brain. When they compared this map to sites on the brain surface that work for noninvasive brain stimulation, the two matched up.
“It’s a beautifully synthetic study,” says George Mark, a pioneer of the use of rTMS in psychiatry at the Medical University of South Carolina who was not involved with the study. “We’ve always wondered how much we really know about any of these brain stimulation treatments. The study looks at invasive and noninvasive techniques like a jigsaw puzzle, and finds out where they match up.”
Sarah Lisanby, chair of psychiatry at Duke University Medical School and a brain stimulation researcher, called the approach “significant”, but expressed concerns about the level of efficacy the evidence pointed to. Besides fMRI, she thinks other measurements of neurological fluctuations may be important to take a look at.
Fox acknowledged the findings do not actually verify the map of connections they’ve drawn up: “It’s a retrospective review of the data we have thus far.” But he’s eager to follow up on this study soon with real data. “We actually want to test it and see if we’re right!”
Fox and others are hopeful the findings can be used to help psychiatrists determine when invasive or noninvasive techniques are more appropriate, and how they can be administered most effectively. Mark believes the study—and the marriage of technology and neuroscience in general—is “part of a larger goal to be able to permanently modify brain circuits” in a way that will completely cure many psychiatric diseases. “Until we figure out how to permanently affect brain, it’s unlikely either of these techniques will replace one-another."