Psychiatrists make life-altering decisions on the basis of a subjective assessment of a set of symptoms. But many freely admit they have far too little information to answer some critical questions: Is the patient suffering from severe depression, or is this a case of bipolar disorder that hasn’t fully manifested itself yet? Will this schizophrenic patient respond to this drug? Draw the wrong conclusions about a depressed patient and the treatment may send him careening into mania. Make the wrong assessment of a schizophrenic person and you may give him an ineffective drug whose side effects could kill him.
“I make these decisions every day,” says Dr. Gary Hasey, associate professor of psychiatry at McMaster University, in Hamilton, Ont., Canada. “If you make an error, you stand a good chance of making things worse.”
Today’s method of choosing treatment—essentially an informed version of trial and error—costs an extra US $8500 per patient per year for the most difficult-to-treat depression patients in the United States. What’s worse, it can eat up years of a patient’s life with fruitless drug therapy, sullied with side effects.
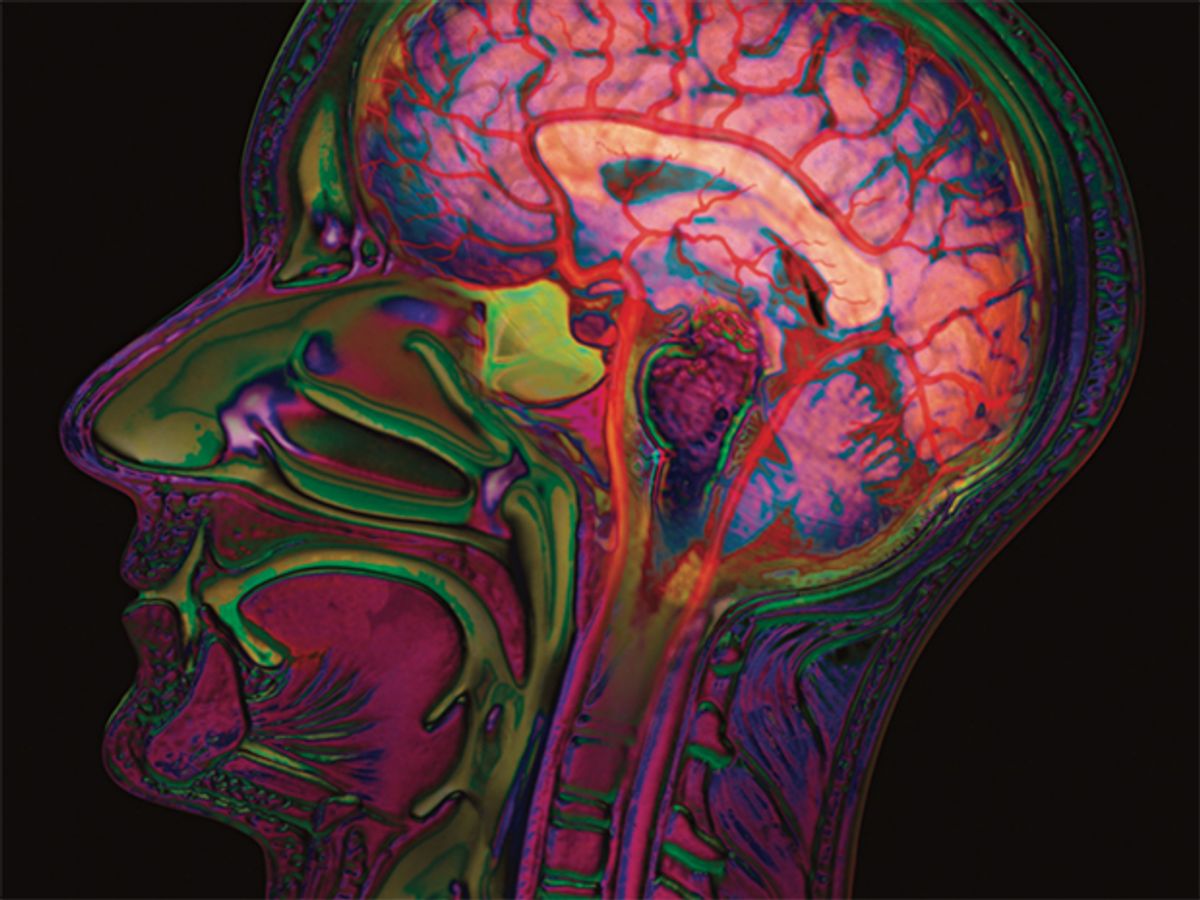
Hasey is among a growing group of psychiatrists pushing for a better way to make those decisions, by using physiological signals that include electrical, functional, and structural data gleaned directly from their patients’ brains via electroencephalogram (EEG) and magnetic resonance imaging (MRI).
With McMaster electrical engineering professor James Reilly and other colleagues, Hasey has been testing software that sifts through schizophrenia patients’ EEGs to find signs that show whether or not they will respond to clozapine, the “drug of last resort.” Other algorithms they have developed can automatically sort people—with an 85 percent success rate—according to whether they suffer from depression, bipolar disorder, schizophrenia, or are free of mind or mood problems. And the group is also developing a system that predicts which of the many available treatments would be most effective for a patient suffering from major depression.
The McMaster group is not alone. Engineers and physicians in the United States and Europe are using MRI brain scans to diagnose schizophrenia and other conditions. And a start-up firm, CNS Response, in Aliso Viejo, Calif., has completed clinical trials of an EEG-based system to aid psychiatrists in predicting which type of depression medication a patient will respond to.
Doctors working with CNS Response recently reported that its EEG-analysis system could predict, with 65 percent accuracy, whether depression patients who had not improved with at least one drug treatment would respond to the next drug tried. Sixty-five percent might not seem like good odds, but it’s a big improvement over the best practices uncovered in a landmark seven-year study, called Sequenced Treatment Alternatives to Relieve Depression. “STAR*D was a high-water mark for serial trial and error,” says George Carpenter, CEO of CNS Response. “But it wasn’t very high.”
At its heart, his company’s system, called referenced EEG, is a large, anonymized database of EEGs from both healthy and mentally ill people. The records included the patients’ treatment histories—what worked and what didn’t. When a doctor uses the system on a patient, the patient’s EEG is correlated with the collected data using statistical regression methods. The system then generates a list of treatment options and their degree of success in patients with similar EEG features. In the clinical trial, reported in the January issue of Journal of Psychiatric Research, Carpenter says that with the system’s advice, doctors “doubled the chances of getting it right” versus the practices laid out in the STAR*D trial.
According to Carpenter, one of the ways the company hopes to improve on those odds is to move to a machine-learning algorithm, one in which the system is trained on the EEG database to pick out the few really important EEG variables rather than comparing the more than 1000 it deals with now.
That teaching process is the crux of the recent MRI research, and it’s just what the software developed at McMaster does using EEG. “What we’ve done is taken 10 000 features and reduced it down to about 5 or 10,” says McMaster’s Reilly, who presented the team’s research at the IEEE Engineering in Medicine and Biology Society conference last September. Reilly and his colleagues trained two software programs to pick out critical features. One learned to predict the success of depression treatment options with 80 to 85 percent accuracy. The other determined with up to 89 percent accuracy whether or not a schizophrenia patient would respond to the dangerous but effective drug clozapine.
Researchers led by University of New Mexico electrical and computer engineering professor Vince D. Calhoun are hoping to reach end results similar to those of the McMaster group. With IEEE Fellow Tülay Adali at the University of Maryland, Baltimore County, and associate professor of electrical engineering Juan I. Arribas at the University of Valladolid, Spain, he has been developing a machine-learning system that can distinguish between people with schizophrenia and those with bipolar disorder on the basis of functional MRI brain scans. The hope is that such a system would give doctors a head start on treatment, because it can be difficult to tell the difference between the two conditions the first time a patient is seen.
An fMRI scan shows not just the overall structure of the brain but also indicates which parts are active at any time, according to changes in the blood flow to them. Using fMRI data, the system automatically finds brain regions whose activity seems relevant to the diagnosis. It was able to sort bipolar, schizophrenic, and healthy brains with about 70 percent confidence. (It can perform a two-way sort—distinguishing bipolar from schizophrenic, for instance—with 90 percent confidence, but that’s an easier problem.) Calhoun and his colleagues presented the workings of the system in the December 2010 issue of IEEE Transactions on Biomedical Engineering.
Researchers at Harvard Medical School are using the newest flavor of MRI for diagnosis. Called diffusion MRI, or diffusion tensor imaging, it shows how water flows inside the tiny neuronal fibers within the brain. That flow allows the mapping of connections between the brain’s regions. With fMRI you are measuring “the symptoms side of things,” says Yogesh Rathi, an assistant professor and leader of the dMRI team at Harvard Medical School. “We want to know the anatomy.”
That could be important, because although the brain function of medicated patients may be altered in a way that would make diagnosis difficult, it’s unlikely that their anatomy would change.
The Harvard system was able to correctly pick out schizophrenic patients 90 percent of the time, according to research presented at the 2010 IEEE International Symposium on Biomedical Imaging. “Our end goal,” says Rathi, “is to diagnose as soon as possible—even try to predict.”
Researchers believe these systems could get so good at diagnosis that they could act as advisers to primary care physicians, says McMaster’s Hasey. That’s important in places where access to an expert is limited. “Essentially, we have the makings of a virtual psychiatrist,” he says.