Researchers have developed an inhalable artificial coronavirus antibody that they say “straitjackets” the SARS-CoV-2 virus and appears (in laboratory, albeit still non-clinical, tests) to impede its ability to infect.
These early tests, they say, suggest the new therapy is potent and powerful enough to merit clinical trials. The ultimate goal, the researchers insist, would be to make it directly available to consumers, possibly even as an over-the-counter home therapy or preventative measure. They say this inhalable COVID prophylaxis/treatment could ideally be ready for public release as soon as “a matter of months.”
The protein they’ve developed, called mNb6-tri (which they’ve dubbed “AeroNabs”), clamps efficiently and tenaciously atop the spike protein of the SARS-CoV-2 virus, hindering the coronavirus’s ability to infect human cells. And, so far as the researchers have been able to determine, once mNb6-tri locks on to the spike protein, it doesn’t readily come off. That appears to be great news for everyone but the coronavirus.
Spike proteins are the pointy spines poking out of the coronavirus that make the virus particle look like an inflated blowfish or a porcupine with its back up.
Spikes—to the world’s great chagrin and horror in 2020—are very good at latching onto a receptor (called ACE2) on many human cells, opening the door for this viral invader. Once inside a cell, the virus hotwires the cell’s machinery to kick out more viral particles, perpetuating a sometimes devastating, body-wide viral infection.
As it turns out, the antibodies of some mammals (llamas and camels, for instance) consist of simpler proteins called nanobodies. And nanobodies can be both an order of magnitude lighter than COVID and relatively easy to characterize and potentially even engineer on an atom-by-atom basis.
So, if nanobodies were to be pressed into service in the COVID-19 war, the thinking goes, one very potent target could be the invader’s spike protein. That element is such a fundamental component of the coronavirus’s infection protocol that if it were somehow rendered ineffective, the coronavirus’s progress through a human host might be stopped cold, or at least substantially hindered.
Aashish Manglik, assistant professor of pharmaceutical chemistry at the University of California San Francisco, uses nanobodies extensively in his research and has spent much of this year investigating whether his specialty could help fight the COVID-19 pandemic.
For this research, Manglik’s lab began by performing an experiment in natural selection—that is, they produced a randomized sequence of more than two billion nanobodies.
“We first created a pool of DNA sequences, where each strand of DNA codes for a unique nanobody,” Manglik says. After that, he recalls: “We put those DNA sequences into individual yeast cells — similar to baker’s yeast, like what we use for at-home cooking. But the cool thing here is we’ve engineered a method where each individual yeast has a unique nanobody tethered to its surface. So in a test tube full of many billions of yeast [cells], each individual yeast will have a different nanobody on its surface.”
Having done that, the team more or less went fishing, says co-researcher Peter Walter, professor of biochemistry and biophysics at UCSF.
Walter and his research group dropped in a bunch of purified coronavirus spike proteins to the mixture. And because they’d also added a magnetic particle to each spike, when they turned on a magnetic field, they were able to watch as the “fishing lures” rose to the surface with the nanobodies that bound most effectively to the spikes attached.
Some nanobodies held loosely to the spike proteins; others were bound more closely. After a “two- to three-week” whittling process, according to Manglik, the researchers narrowed the pool of two billion candidates down to 20 semi-finalist nanobodies that each appeared to optimize three competing factors. The ideal nanobody would need to: bind quickly and tightly to the spike, remain robust in the presence of heat and other degrading real-world factors, and be as “human-like” as possible. (This last point was necessary to head off any potential complications such as an overzealous human immune system counterproductively attacking the nanobody.)
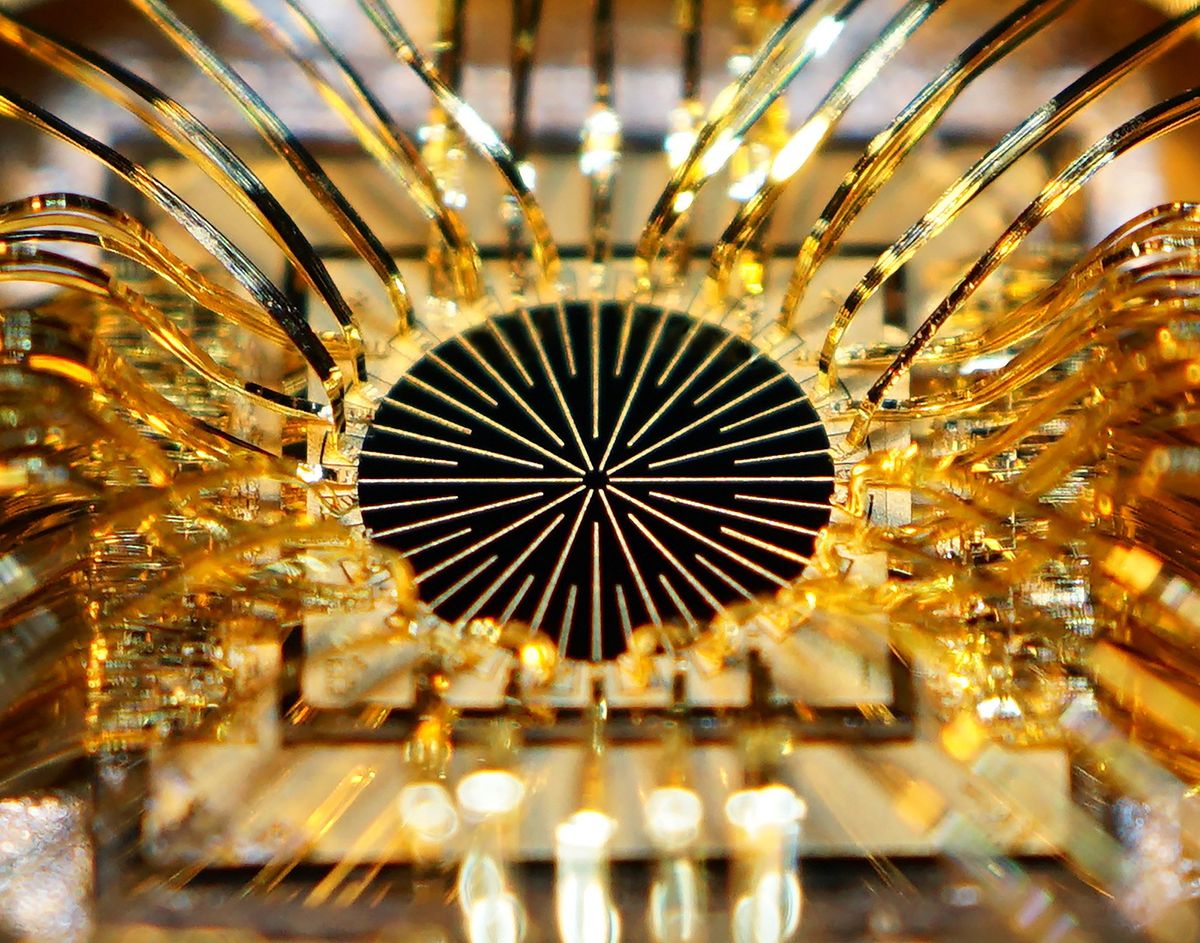
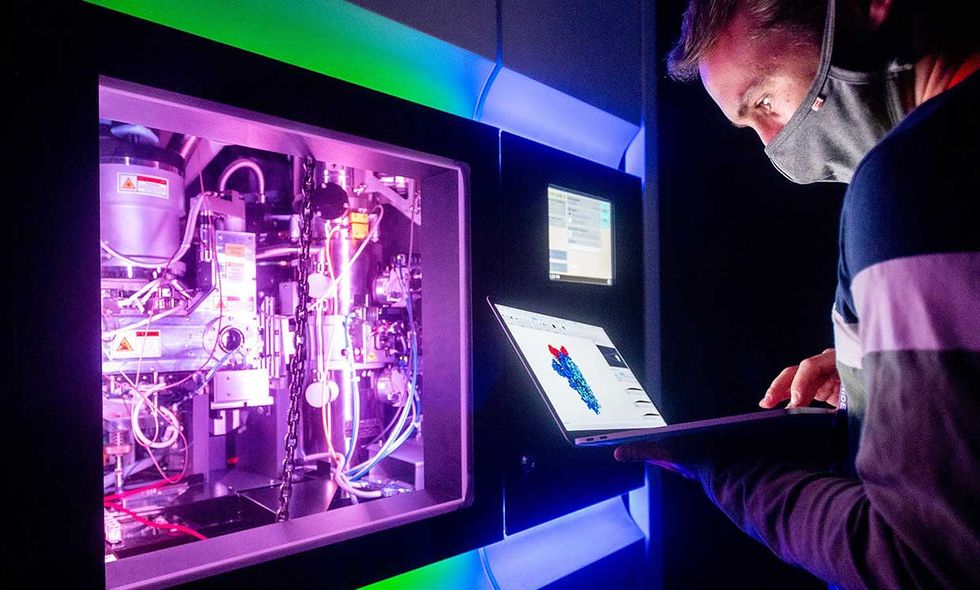
Ultimately, they narrowed the nanobody field down to the best of the entire lot: What they called Nb6. Using a new imaging technique called cryogenic electron microscopy, they studied Nb6 at the atomic scale as it clamped on to the COVID-19 spike protein. The team made adjustments, they say, that improved Nb6’s binding affinity to the spike by another 500 times.
Then, because the spike protein is a trimer (containing three identical proteins), the researchers turned their modified nanobody (mNb6) into a tri-fold nanobody specifically engineered to fit the precise contours of the novel coronavirus’s trimer spike. In other words, they'd now created mNb6-tri.
“This dramatically increases the tightness of binding between this trimeric construct and the spike protein,” says Manglik. “When we did this, we found we got a 200,000-fold gain in the tightness of binding—such that once one of these [AeroNabs nanobodies] binds, it basically never comes off. And we’re at the limit of detection for the kind of instrumentation and the approaches we use to look at how long the molecule, once bound, stays on. We haven’t seen it come off. We think it’ll be bound to that spike protein for weeks if not months.”
Walter said that because the nanobodies are so small and so effective in seeking out and binding to coronavirus particles, he anticipates that one dose of AeroNabs particles per day could be sufficient for testing its effectiveness for COVID-19 prevention or treatment. Walter calls AeroNabs—if its safety and effectiveness can be substantiated in clinical trials—essentially “molecular PPE.”
For patients who already have SARS-CoV-2 in their lungs, Walter anticipates a nebulizer creating an AeroNabs mist, which the patient could inhale. “A few minutes once a day should be sufficient,” he said, to test whether AeroNabs could be effective for COVID-19 patients with serious symptoms.
And because a coronavirus infection often begins in the nasal airways, an AeroNabs nasal spray might also be tested as a preventative measure for front-line workers and other potentially exposed populations as well as people who are positive for the coronavirus but don’t yet show symptoms.
“AeroNabs is stable and easy to produce in industrial quantities at very low expense,” Walter says. “And it can be shipped around the world as a dry powder. So we really hope it will become broadly available to the developing world as well.”
On the question of AeroNabs’ safety, Walter and Manglik point to the precedent of another nanobody therapy—Caplacizumab for the blood disorder TTP (thrombotic thrombocytopenic purpura0—that was recently approved by the U.S. Food and Drug Administration.
Walter notes, too, that the name “nanobody” may be deceptive. AeroNabs, he points out, are not in fact nanoparticles or any such exotic creation of nanotechnology. The mNb6-tri protein consists, by design, almost entirely of the same amino acids that make up human proteins. Human airways and bloodstreams are awash in all kinds of proteins that are much like mNb6-tri wherever one might care to look. Only this particular protein has been engineered specifically to bind, as Manglik says, “absurdly tightly” to COVID’s primary tool for breaking and entering human cells.
For those reasons, the researchers expect toxicity concerns for AeroNabs to be low.
That said, they’re now seeking commercial partners to take on clinical trials to investigate questions of safety and effectiveness against the coronavirus in human patients in real-world clinical settings.
The paper describing the group's AeroNabs research was published last week on the online pre-print server bioRxiv. Walter says that since then, the group has fielded interest from “quite a number of prestigious journals.”
“We are all hoping that an effective vaccine with lasting effects can be developed very fast,” Walter said. “But ramping up the production capacity and distribution capacity will take a while. And before that becomes available around the globe, we hope AeroNabs could act as a stopgap measure.”
This article appears in the October 2020 print issue as “Engineered Antibody Mist Blocks Coronavirus.”
Margo Anderson is the news manager at IEEE Spectrum. She has a bachelor’s degree in physics and a master’s degree in astrophysics.