Sweat analysis isn't new: the dynamic chemical composition of perspiration has inspired researchers from elite athletic performance specialists to chronic disease experts to try to decipher its signals.
But translating raw perspiration into "sweat equity" in real time in everyday life is not an easy task. Sometimes climatic conditions don't lend themselves to creating enough sweat to analyze. Sometimes the heightened level of activity necessary to get enough sweat produces chemical changes in the fluid that aren't indicative of a subject's true state. And sometimes, a person is physically unable to create sufficient sweat volumes to analyze with existing technologies.
This problem is especially challenging in the study of stress response in "normal" routines or among those rendered inactive with chronic diseases. Cortisol level is one widely accepted principle in gauging the amount of physiological and cognitive stress someone is experiencing at a given time, but it has been hard to translate that principle into practice outside controlled conditions.
A highly accurate yet comfortable sensor, now in proof-of-concept trials on human subjects in real-world conditions, might be a critical component of systems that will successfully address those obstacles.
Reading off a person's glucose and cortisol levels is the goal. Fortunately, sweat sensors may yet be up to the job.
The technology, developed by Dallas-based EnLiSense LLC and the University of Texas at Dallas, is promising enough that the U.S. government's Biomedical Advanced Research and Development Authiority (BARDA), featured it in its July 2021 innovation highlights. The patch, just 120 square millimeters, can detect target biomarkers in sweat volume as low as 1 to 3 microliters.
Same but different as CGM
Continuous glucose monitoring (CGM) devices such as the Abbott Freestyle Libre and Dexcom G6 might be the most familiar examples of real-time microfluidic monitoring. EnLiSense CEO and co-founder Sriram Muthukumar explained EnLiSense's technology and marketing strategy in comparison to them.
CGMs work, he says, by analyzing changes in interstitial fluid surrounding the body's cells. They do not measure blood glucose directly.
"They use a microneedle that penetrates the skin and uses capillary action to harvest interstitial fluid around the vein," Muthukumar says. "So if the value of the blood glucose is x, the value of the interstitial fluid will be y. I don't care about the absolute values as long as I can predict the trend of the change in x to the change in y. The CGMs use the changes in y to say whether you are in a green zone or not, like driving in a lane. Are you steering too far right or left, are you getting into a hypo- or hyperglycemic state?"
The premise behind the EnLiSense sensor, branded the SweatSenser, is the same, he said. However, CGMs measure that gradient as a current through a kind of electrochemical process called amperometry—in which ions in solution are detected electrically. And this amperometry trick works for sensing glucose, Muthukumar says. But for substances that do not carry a charge or have a minimal charge, cortisol among them, Muthukumar says such an approach does not work.
So the EnLiSense sensor uses an application of Faraday's law of induction that harnesses electrical measurements to infer chemical properties of a system, called electrochemical impedance spectroscopy (EIS). EIS can employ two types of sensors—either a faradaic sensor, which uses reduction/oxidation (redox) reagents in its electrolyte solution, or a nonfaradaic sensor, which does not. The EnliSense cortisol sensor uses the nonfaradaic approach, because it allows for the detection of subtle changes in biomarker levels at very small volumes.
The sensor, which can be worn on a watch-like strap or other non-obtrusive device, is also capable of housing detection strips for more than one target at a time, and has no microneedle that can cause discomfort, such as a CGM.
Complementary closed-loop research
University of Houston researcher Rose Faghih is eager to have access to the EnLiSense sensor. Faghih is running experiments on stress reaction and control using skin conductance response (SCR), the measurable result of electrical characteristics derived from the change in sweat gland activity as stressors change. Faghih is investigating closed-loop systems that can infer cognitive stress levels and offer real-time behavioral suggestions. For instance, she says in a smart home setting, a closed-loop system could measure a resident's stress levels and correspondingly change the level of light or music to suit their mood. Having real-time cortisol sensor data to add context to SCR data would be a boon to her research, she says.
There are even indications this technology could unlock new kinds of treatments for obesity.
"I focused on analyzing cortisol data during my Ph.D. and have a lot of experience with it," she says. "All the cortisol data I have worked with is basically blood samples taken every 10 minutes. I very much hope these will become commercially available, or available through collaborations so I can work with these researchers and use cortisol to infer more information about the brain state."
The EnliSense has already been successfully tested in simultaneous detection of cortisol and glucose in a typical workday scenario on 10 subjects in EnLiSense co-founder Shalini Prasad's UTD labs. The interaction of the two substances might unlock treatments for obesity; Faghih has done similar work on the interactions of cortisol and leptin.
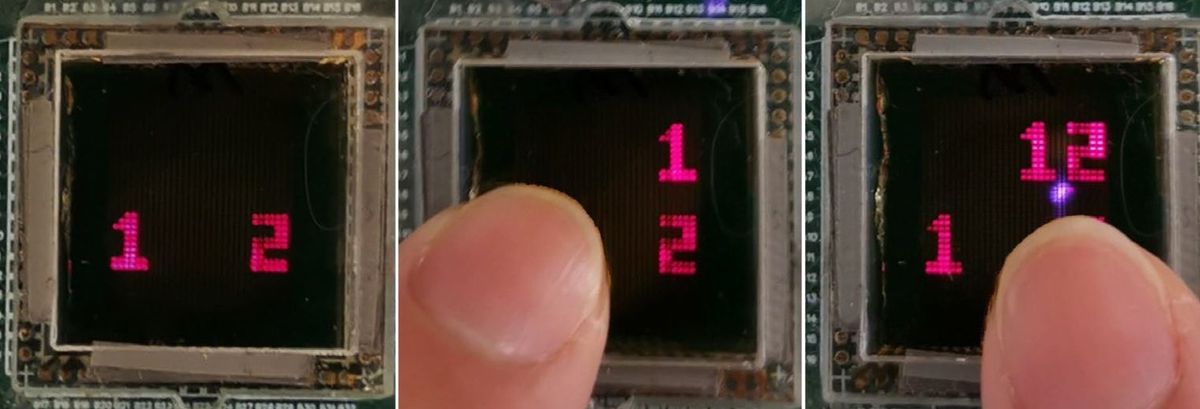
Don't Sweat It! Passive Sweat Detection for Continuous Metabolitewww.youtube.com
Real-world diagnoses will mandate these multi-marker capabilities, Muthukumar says, but might also provide a vital reference point versus the already widely used CGM technology as the company ramps up its market strategy.
"The FDA panel will look for a predicate," he says. "The platform can do more than glucose, but that glucose measurement assures us we can do a reference correlation to Abbott's platform. When I looked at the documentation on which they got FDA approval, that data is so noisy. I'm very confident that I can ask the FDA, 'If you approved them, what is stopping you from approving me?'"
- Sweat Sensors Will Change How Wearables Track Your Health ... ›
- New Wearable Sensor Detects Stress Hormone in Sweat - IEEE ... ›