Could you perceive the touch of an ant’s antenna on your fingertip? This new tactile sensor can, and its inventors report that it could one day be integrated into prostheses to give wearers a superhuman sense of touch.
The sensor converts pressure from touch to electric signals that, theoretically, could be perceived by the brain. Researchers at the Chinese Academy of Sciences in Ningbo, Zhenhai, described their invention yesterday in the journal Science Robotics.
There have been a lot of touch sensors described in the literature, but this one’s sensitivity is off the charts. It perceives the most subtle touches, including wind, tiny drops of water, and the actions of an ant. In tests of the device, when the ant wasn’t walking, the tactile sensor even detected the touch of the insect’s antenna.
In numbers, that’s a sensitivity of 120 newton-1, a detection limit of 10 micronewtons, and a minimum loading of 50 micronewtons, or 1.25 pascals—less than the sensing threshold of human skin. “That’s a very sensitive sensor,” says Nitish Thakor, a biomedical engineer at Johns Hopkins University, who was not involved in the study.
The inventors of the sensor, led by Run-Wei Li, at the Academy’s Ningbo Institute of Materials Technology and Engineering, accomplished the feat by applying the physics of giant magneto-impedance (GMI).
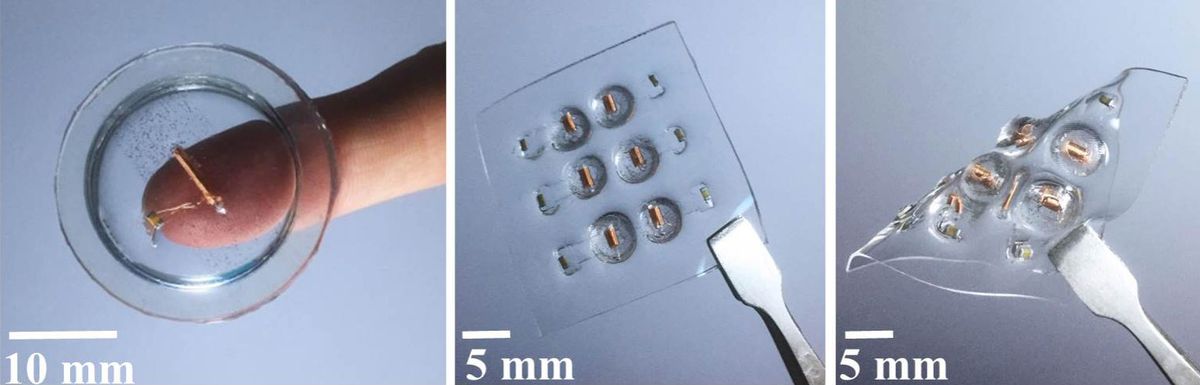
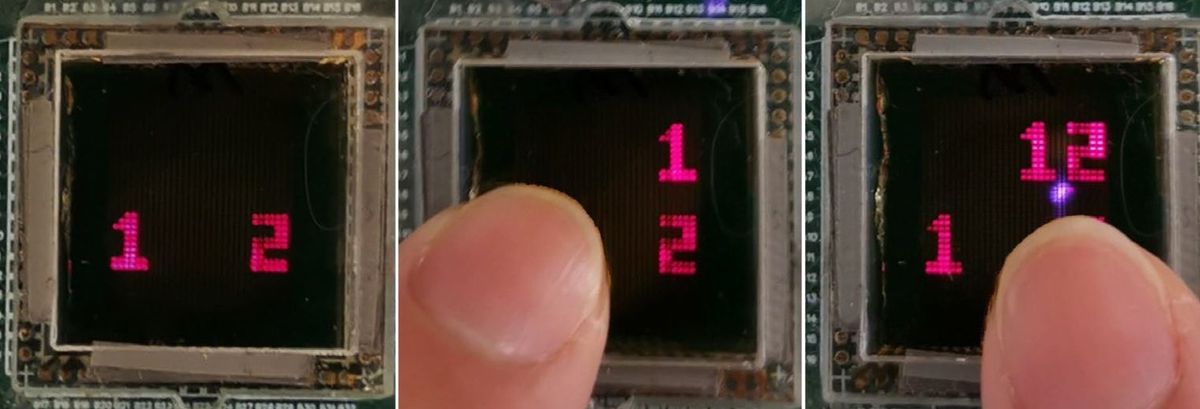
The sensor is composed of a polymer membrane with magnetic particles on its top surface and a magnetic sensor integrated inside, along with an air gap. When pressure is applied to the surface, the membrane deforms inward, causing the magnetic particles on the top to move toward the inductive magnetic sensor on the inside, which is made of giant magneto-impedance material. As a result, magnetic flux passing through the inductive sensing element increases, and impedance of the sensing element decreases. An oscillation circuit composed of an inductor and a capacitor are applied in parallel, and used to convert time-domain signals into frequency-domain signals.

Run-Wei Li’s group “has created a clever circuit that produces a rate code in response to pressure,” says Thakor. “Our nerves send a message from our skin to the spinal cord to the brain as these spikes. It doesn’t send it as a 16-digit computer code, and it doesn’t send it as an analog signal. It sends it as a rate code. So it’s a nice first step.”
But the device falls short in several ways, says Thakor. For one, “the oscillations are not truly mimicking nerves,” he says. Hacking into the body’s sensory encoding requires a significant amount of recording of actual nerve impulses, and lots of experimentation to understand the sensations created by artificial stimulation. When we touch something and our sensory nerves perceive it, what does that look like in electrical signals? What are the patterns of electrical pulses that communicate with our brains?
The authors did not investigate this, at least in this paper, nor did they integrate the device onto a prosthetic or hook it up to the body’s communication system. “An engineer or sensor designer may like it, but a neuroscientist would be critical,” says Thakor.
Second, while the sensor array is flexible, the sensors are crude in size—about 5 millimeters in diameter, which isn’t practical for a prosthetic hand. Third, the sensors register only the really subtle sensations. Stronger pressure would saturate them, so the sensors don’t capture the full range of human touch, says Thakor.
IEEE Spectrum was not able to reach the authors of the new paper for comment.
Many groups are working on improving the electrical connections between prosthetics and the human body, in an attempt to improve the experience for people with bionic limbs. Earlier this year, Thakor and his colleagues reported a multilayered electronic skin that enabled a prosthesis to perceive and transmit the feeling of pain to its gracious human volunteer. To do this, the scientists first had to determine the stimulation patterns needed to elicit pain in the phantom hand of the volunteer, and then recreate that with pulses generated by a computer model of the nerve signals.
Zhenan Bao’s group at Stanford in 2015 reported a flexible organic transistor circuit that transduces pressure into digital frequency signals. And Dustin Tyler’s team out of Case Western Reserve University, in Cleveland, developed a neural interface that gave two volunteers with upper arm amputations the sensation of touch in phantom hands. The device lasted for over a year.
Run-Wei Li’s group has made an awesome sensor that has the potential to communicate with the human body. Now lets hope researchers take it to the next step and connect it to a prosthetic that amputees can actually use.
Emily Waltz is a features editor at Spectrum covering power and energy. Prior to joining the staff in January 2024, Emily spent 18 years as a freelance journalist covering biotechnology, primarily for the Nature research journals and Spectrum. Her work has also appeared in Scientific American, Discover, Outside, and the New York Times. Emily has a master's degree from Columbia University Graduate School of Journalism and an undergraduate degree from Vanderbilt University. With every word she writes, Emily strives to say something true and useful. She posts on Twitter/X @EmWaltz and her portfolio can be found on her website.