The COVID-19 epidemic in China was gathering terrible force when 11 overworked Chinese physicians found time to write a research paper. At the time, in mid February, confirmed cases of the disease were inching towards 60,000 and the death toll stood at nearly 1,400. The doctors, most of them pulmonary specialists at the Xi’an Chest Hospital, had already treated scores of people seriously stricken with the disease.
Weary as they were, they had something they wanted to tell the world: “Ultrasound is playing an indispensable role in the diagnosis, treatment and efficacy evaluation of severe acute pneumonia,” the life-threatening illness associated with the most severe cases of COVID-19.
Medical ultrasound, which provides instant, full-motion video of a cross-section of the patient’s body, is of course well known for its role in fetal imaging. It’s also frequently used to image organs such as the heart, liver, gallbladder, and kidneys. Lung ultrasound is a relatively recent medical technique, dating to pioneering work by Daniel A. Lichtenstein in France and described in a research paper published in 2008.
Now, with COVID-19 cases worldwide surpassing 2.5 million and the death count standing at more than 176,000, lung ultrasound has emerged as a top medical tool in the global struggle against the disease. Hospitals are using it to monitor and even diagnose cases, particularly in places where tests are scarce or unavailable. They’re relying on it to decide who gets into hospital emergency rooms, and who will go to the intensive-care unit.
Intriguingly, as their front-line systems, many hospitals are relying not on their biggest, most sophisticated systems—stationary or cart-based machines that can cost between US $50,000 and $100,000—but rather on handheld, pocketable systems that cost a tenth as much or less.
Philips, GE, Siemens, Canon, and a couple of startups, Butterfly Network Inc. and Clarius Mobile Health, are key suppliers of the handheld ultrasound systems, which began proliferating in the medical community only about 10 years ago. These pocket-size systems consist of a transducer, which is held against the patient’s body and is about the size and shape of a small electric hair trimmer, which plugs into a smart mobile device, such as a smartphone or a tablet.
“We are selling them as quickly as we can make them,” says Anthony Gades, director of clinical science at Philips Point-Of-Care Ultrasound in Bothell, Washington. “We’re seeing huge orders from healthcare systems.”
It’s a surprising turn for the medical imaging technology. Because ultrasound is quickly dissipated in air, the technique was for years thought to be of little use for studying the lungs. “Ultrasound is not a natural candidate, you might think, to assess the lungs,” says Mathias Goyen, chief medical officer, Europe, for GE Healthcare. “But here, dealing with the pandemic, all of a sudden ultrasound really has a great place, a great role. You can use it in the ICU, you don’t have to bring the patient to the radiology department. It’s inexpensive; it’s available; it’s a bedside test. There’s a huge, huge demand.”
Ultrasound’s indispensability in the current crisis starts with the fact that it can quickly and easily spot the viral pneumonia associated with the most serious cases of COVID-19, says Cindy Owen, director of clinical insights and development for GE Healthcare’s Point-of-Care Ultrasound.
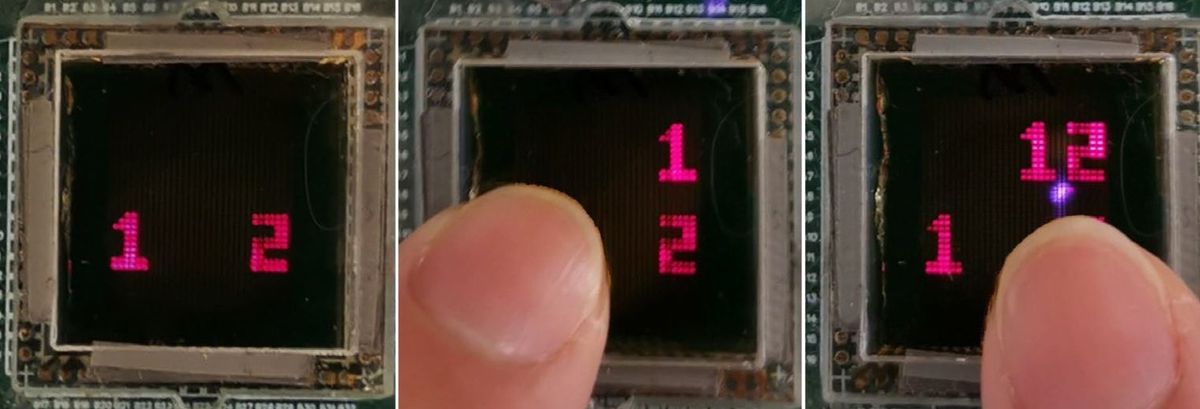
Critical Case: A lung ultrasound scan of a patient with advanced COVID-19 shows characteristic signs. In this video, recorded using a GE Vscan Extend handheld ultrasound unit, an irregular and thickened pleural line is visible as bright horizontal layers near the top. Radiating down from them are B-lines, which are also beginning to thicken and consolidate into a wide smudge—an indication of substantial fluid in the lungs.Video: GE Healthcare
In examining a lung, physicians begin by looking for the pleural line, a bright streak in the image that corresponds to the pleura, the layered sheet of tissue that envelops the outside of the lungs and encloses the chest cavity. “You look at the pleural line,” Owen explains. “If the lungs are normal, you see equidistant horizontal lines called A lines. But if there’s fluid,” an indication of pneumonia, “you see bright streaks that move with the patient’s breathing, called B lines.” As the pneumonia becomes more serious, the B lines merge in some places into what are called coalesced, or confluent, B lines, and the pleural line appears thickened.
On ultrasound, the lungs of patients seriously infected with COVID-19 show up with a characteristic variegated pattern. “That pattern—the pleural thickening, the B lines, and confluent B lines, in a distribution that is patchy and bilateral, that is, for me, COVID until proven otherwise,” says Bilal Jalil, an intensive-care and pulmonary physician in the Dallas, Texas area.
These ultrasound indicators of COVID are so characteristic that some doctors are now using ultrasound as a kind of provisionary test for the disease. The most accurate chemically-based diagnostic test, which makes use of polymerase chain reaction, is still scarce in some places, takes days to deliver results, and has been plagued with false negatives. Many hospitals in COVID hotspots are foregoing the test, at least initially, and using handheld ultrasound as a literal front line. Using the handheld systems, they’re examining patients’ lungs to determine whether they should be admitted and if so, whether they need intensive care.

The huge demand for the handheld machines isn’t hard to understand, according to Philips’s Gades. “Because they’re so small, you can put a sheath around the entire system to prevent any pathogens from contaminating it,” he explains. “Then you discard the sheath in between patients. That size advantage is huge now.”
Jalil explains that the portability enables him to minimize his—and other people’s—visits to infected areas. “If I have an intubated patient who’s in the ICU,” he says, “I’m going to go in, and I’m going to take my machine with me. Maybe I have to put a central line in. Maybe I have to do a procedure on that patient. Maybe I just need to go and examine that patient. I’m not going in a second time just to do an ultrasound. I just take it in with me, and do everything I need to do in that one episode of care. Once I’m done with that, I come back out with all the answers I need.”
Another plus of ultrasound, he notes, is that unlike X-rays, there is no potentially harmful ionizing radiation, meaning that doctors can use the devices every day to closely track the course of the disease.
A major trend in medical ultrasound, reflecting advances in medical imaging in general, has been the integration of smart software and apps, including ones based on artificial intelligence. The COVID-19 crisis seems set to accelerate many of those initiatives. “Believe me, AI is the number one priority for most imaging devices,” says Jalil.
These apps and software are typically aimed at assisting relatively inexperienced users as well as helping veterans work more quickly and consistently. Gades points out that the Philips handheld, connected to a smartphone, enables the user to stream live video from the phone’s front-facing camera as well as the transducer to an observer anywhere in the world, who can offer pointers on transducer placement and other subtleties. Regarding AI and other advanced software, he says, “we’ve been devoting tremendous resources to making this even more usable for those with little training.”
He adds, “we’re actively partnering with the [U.S. Department of Defense] as well as many medical centers to develop automated ways to address these types of situations.”
GE already has an AI-based software lung tool for its larger, cart-based Venue line of ultrasound machines. It automatically counts B lines and consolidations in imagery and uses the data to calculate a lung “score” indicating the seriousness of an infection. The company is also working on advanced apps for its handheld systems, which are called Vscan, according to Nahi Halmann, chief engineer for GE Point of Care Ultrasound. The current surge of use in the pandemic will turbocharge those efforts, Halmann adds: “Groups are collecting data, and this will lead to new ideas about how to develop future technologies.”
Glenn Zorpette is editorial director for content development at IEEE Spectrum. A Fellow of the IEEE, he holds a bachelor's degree in electrical engineering from Brown University.