THE INSTITUTE COVID-19 patients can find it difficult to breathe as the virus infects the upper or lower parts of their respiratory tract. Severe cases result in edema—a build-up of fluid—and gas exchange failure in the alveoli, the small air-containing spaces in the lungs that exchange oxygen and carbon dioxide molecules with the bloodstream.
Respiration being an absolute requirement for life, it is not surprising that the mechanical ventilators found in intensive care units have been in great demand during the past few months. These devices use a mobile compressor to assist with the patient’s breathing by pushing air through a tube placed in the trachea to expand the lungs.
The need for mechanical ventilators has far outpaced the number available. There are many efforts to address the supply shortage. For example, some car companies, such as General Motors, have adapted existing designs of ventilation equipment and are manufacturing them at their facilities. Established ventilator manufacturers have increased production while also making some of their designs freely available so that others can reproduce them.
While these endeavors aim to produce ventilators that are closer to the current standard medical equipment used in ICUs, we are also seeing a wave of interim DIY devices being developed to increase the supply. These rapidly scalable, low-cost emergency ventilators (EVs) are mainly the automated version of manual bag-based resuscitator devices, commonly known as Ambu bags or bag valve masks (BVMs).
These small, compact, balloonlike bags have a soft air reservoir that can be squeezed by medical professionals to inflate a patient’s lungs. Oxygen is administered via tubing to this bag. Exhalation occurs due to elastic recoil of the patient’s chest, and the bag resumes its original shape. BVMs can theoretically support a patient indefinitely, but in reality, it is a temporary measure as manual compression is tedious and lacks good control.
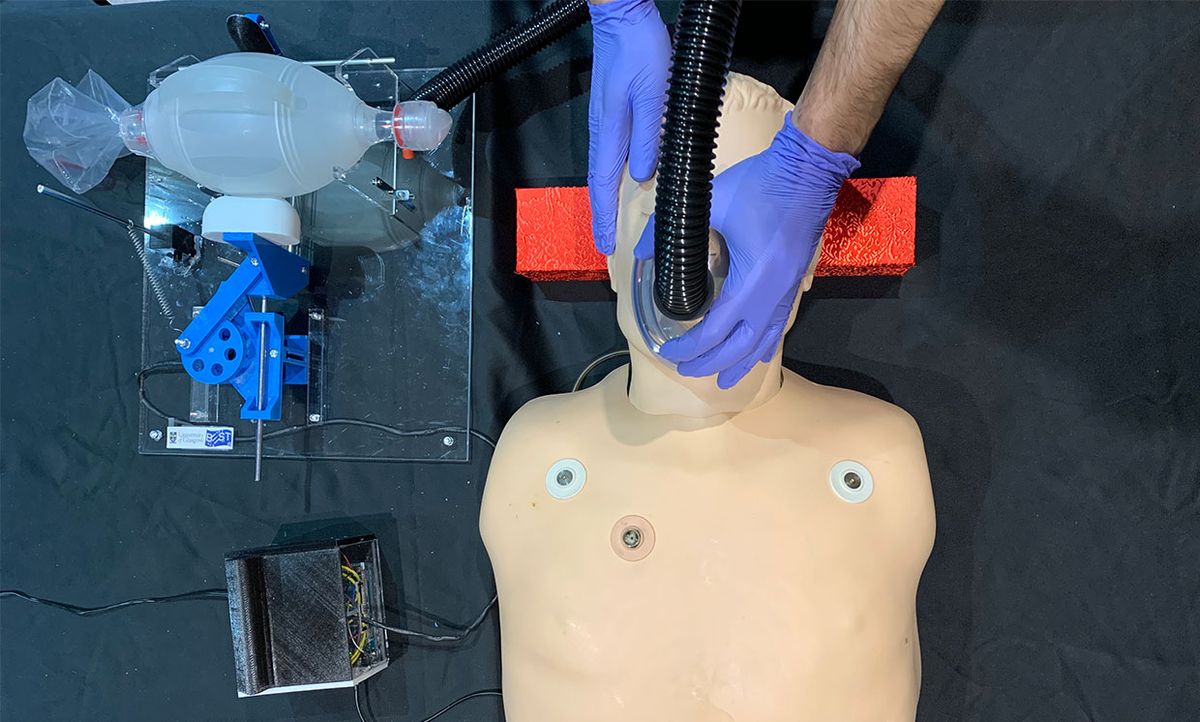
The DIY emergency ventilators address this issue by automating the squeezing of the bag. They are open source and typically built using off-the-shelf parts, widely available materials, and simple fabrication and assembly techniques. A few examples include MIT’s E-Vent, Oxford University and King’s College London’s OxVent and University of Glasgow’s GlasVent.
Almost all use a motor or air compressor to squeeze the BVM. The motor’s speed and the air compressor speed controls the breathing rate, and the plunger controls the level of BVM compression. The amount of compression determines the tidal volume—the volume of air entering and exiting the lungs after each breath.
The attributes of these initiatives are their fast deployment, scalability, simple assembly, compact size, and low cost. The devices are meant to be used only for short periods of time—up to a few hours. The GlasVent offers an additional feature: It can be operated manually by someone with little to no medical experience.
This how-to video shows how to manually operate the University of Glasgow’s GlasVent respirator.
These EVs offer some of the same features as mechanical ventilators and could be quite useful in emergency situations where the availability and cost of standard ones is limiting. The cost per mechanical ventilator averages anywhere from US $20,000 to $100,000, which by no means makes it a cheap intervention. On other hand, the cost of EVs could range from $100 to $1,000.
In addition, because they can be powered through the main supply, batteries, or manually in the case of GlasVent, EVs can be used during power outages. Also, their compact size allows them to be used in ambulances, medical transportation vans, and even in cars.
Even though they may seem relatively simple from an engineering perspective, designing a ventilator that can be used safely and reliably to help a person breathe is a significant challenge. To help those who intend to develop DIY EVs, it’s important to know some fundamentals.
BREATHING BASICS
Ventilators are designed around a few fundamental respiration parameters, including tidal volume (air volume entering and exiting the lungs each breath), airway pressure, and the respiratory rate. The control of airway pressure is important as excessive volumes or pressures can stretch lung tissue, causing barotrauma injury.

There are four distinct measures of airway pressure during a typical ventilation breathing cycle [right]. Positive end-expiratory pressure (PEEP) helps the ventilator maintain air in the lungs at the end of a breath, preventing the collapse of alveoli and, at higher levels, improving gas exchanged. Peak inspiratory pressure is the maximum airway pressure during inspiration. Plateau pressure represents the pressure in the alveoli at some particular phase of breathing and is often used as a gauge to determine the maximum pressure that can be applied. Driving pressure is the plateau airway pressure minus PEEP. It can also be expressed as the ratio of tidal volume to respiratory system compliance, indicating the decreased functional size of the lung observed in patients.
These measures of airway pressure provide the extremes of both inspiration and expiration.
The respiratory rate (number of breaths per minute) is another important parameter. It is commonly around 16 to 20, each breath lasting approximately three to four seconds, but it may need to be increased to 30 to 50 in extreme cases such as COVID-19, where gas exchange is compromised.
VENTILATION BASICS
There are many ways to supply ventilation to a patient. Depending on the patient’s breathing efforts and sedation and the pressure or volume control, the ventilation can control the breathing entirely or just provide additional assistance.
Optimal ventilator parameters vary among patients and can change for each patient during the course of a disease. When patients begin breathing more independently on their own, the ventilator’s parameters must be adjusted so the machine doesn’t continue to push air into the lungs at the same rate.
For these reasons, operating mechanical ventilators can be complex for anyone with a nonclinical background. Clearly, there is need for trained professionals, which typically includes intensive care physicians, anesthesiologists, intensive care nurses, and respiratory therapists. Some training for EVs is needed, too, even if they are used only to provide basic control over the pressure and volume of air in the lungs.
Typically, putting a patient on a mechanical ventilator requires the insertion of a laryngeal mask, endotracheal tube, or tracheostomy. Such forms of invasive ventilation require a patient to be sedated, which can lead to complications such as blood clotting and the need for dialysis.
Ventilation can also be accomplished noninvasively, using an airtight face mask, but it carries other risks, such as blowing air into the stomach, poor airflow, and the possibility that fluid or solid particles might end up in the windpipe or lungs. For these reasons, noninvasive ventilation is not recommended with mechanical ventilators other than for short-term assistance in the form of mild PEEP in a conscious patient.
It may be more suitable for EVs because they are meant to complement mechanical ventilators for a short period.
These same risks apply in the case of EVs, but they are intended mainly to provide noninvasive ventilation and are to be used for a short period of time, up to 100 hours. This buys the COVID-19 patients with temporary breathing issue some time. Often, their immune system successfully fights the virus.
EV OPPORTUNITIES AND CHALLENGES
Using an Ambu bag as the backbone of a DIY EV has several merits. Such manual resuscitators are widely available, and most hospitals have them in stock. They have already been tested and certified for medical use, making them suitable for sterilization. The bags are also compatible with a variety of equipment, such as masks, valves, intubation equipment, filters, and oxygen supply.
Some BVMs come with safety features, such as pop-off valves, therefore simplifying the rest of the design. One drawback of using BVMs to meet COVID-19 needs is the risk of aerosolizing the virus, because exhaled air is not collected.
EVs must receive regulatory approval from agencies such as the U.S. Food and Drug Administration before they can be deployed.
But once approved, they could potentially be used beyond just mitigating the current COVID-19-related supply shortage. EVs could ultimately become a household medical device, like the pulse oximeter. Many people with a variety of medication conditions use this chip-clip-like device on their finger to check their blood oxygen level and heart rate.
With training from a medical professional, patients with asthma could use such small, portable ventilators for breathing treatments to open up blockages in small air passages. EVs also offer an attractive and affordable alternative in many resource-poor settings. In low- and middle-income countries that lack costly mechanical ventilators, an EV may be a patient’s only option. Given this, basic EVs, at much lower costs, can make a huge difference in people’s lives.
This article appears in the September 2020 print issue as “Why DIY Ventilators are Still a Vital Stopgap.”
Ravinder Dahiya is an IEEE Fellow and a professor of electronics and nanoengineering with the Bendable Electronics and Sensing Technologies group at the University of Glasgow’s School of Engineering, in the United Kingdom. Dahiya is also the president-elect for the IEEE Sensors Council. Andrew Hart is a hand and plastic surgeon at the Glasgow Royal Infirmary, NHS Greater Glasgow and Clyde.