Moderna, the company behind one of the best-selling COVID-19 vaccines in the world, is trying to prove that its messenger RNA (mRNA) platform is not a one-trick pony.
Earlier this month, the biotech firm announced that an experimental mRNA therapy, called AZD8601, was well tolerated and showed hints of efficacy when injected directly into the hearts of seven people undergoing coronary artery bypass surgery.
It was the first demonstration in Moderna's 11-year history that the company's mRNA molecules could safely produce functional proteins that directly exert a therapeutic effect inside the body.
"The results are very encouraging," says Lior Zangi, a heart regeneration researcher at the Icahn School of Medicine at Mount Sinai in New York whose 2013 paper formed the basis for AZD8601. "This is the right tool for this dreadful disease."
But according to Zangi, mRNA "is not an answer for everything." And in fact, the concept of using mRNA as a drug to treat established disease, rather than as a preventative measure to ward off viral infections, is probably not a viable approach in many disease settings.
In 2015, Moderna planned to move 100 mRNA drug candidates into clinical trials within a decade. Vaccines were hardly mentioned.
When only limited amounts of protein are needed for a short time to heal damaged tissue, mRNA can get the job done—think muscle repair following a heart attack, or neural recovery after a stroke. Genome-editing companies such as Intellia Therapeutics are also turning to mRNA to deliver components of the CRISPR-Cas9 machinery for one-and-done gene therapies in people with inherited DNA defects.
"It's a come-and-go technology," Zangi says.
For most everything else, mRNA technologies—at least in their current form, experts say—are not up to snuff. "There's a reason why [most companies] are only doing vaccines," says Robert Kruse, a physician-scientist and biotech entrepreneur at Harvard Medical School in Boston.
Those arguments run counter to Moderna's long-running narrative as a platform company capable of deploying its mRNA for almost any ailment.
When I first met the company's CEO Stéphane Bancel at his Kendall Square offices, back in April 2015, he laid out a boldly ambitious plan: to move 100 drug candidates into clinical testing within the next 10 years, using mRNA to treat everything from cancer to rare genetic diseases.
"We are developing an OS of mRNA," Bancel told me at the time. "This is a true platform"—but one he intended would fix rather than prevent disease. Vaccines were hardly mentioned in Moderna's early press and public presentations.
Fast-forward two-thirds of a decade and Bancel's brash plan has largely fallen through. Faced with the many challenges involved with transforming mRNA technologies into therapeutics, the company opted to pivot to vaccines instead.
Rather than developing mRNA drugs that could replace missing or deficient proteins to treat chronic diseases—as Bancel initially proposed—Moderna is now largely a vaccine maker, with most of its clinical pipeline devoted to prophylactic measures for respiratory and mosquito-borne viruses.
Moderna has now forged ahead with early-stage trials for autoimmunity, enzyme deficiency disorders, and cancer.
Industry insiders have traditionally seen such products as less transformative and lucrative.
And if it wasn't for a global pandemic yielding a megablockbuster vaccine, Moderna might still be struggling to convince investors of its platform's value. It definitely wouldn't be valued at more than $100 billion, the highest of any biotech company founded in recent decades (and far exceeding that of any other drugmaker with only a single marketed product generating revenue).
For companies like Moderna, the COVID-19 response showcased the speed, flexibility, and nimbleness of their mRNA platforms. With vaccines, just a few injections of low-dose mRNA yielded sufficient levels of viral protein to kick the immune system into gear.
To tackle a lifelong health condition, however, any mRNA drug would have to make bucketloads of protein. Yet, the short-lived nature of the molecule, along with its attendant side effects, currently precludes administering repeated doses of mRNA on any schedule capable of having a therapeutic effect.
New startups are in works to address these challenges. And Moderna, while mostly focused on vaccines, has forged ahead with early-stage trials involving a few product candidates for autoimmunity, enzyme deficiency disorders, and cancer.
But it has also quietly abandoned several other therapeutic programs—recently shelving, for example, mRNA-based drug candidates for Fabry's disease (a rare inherited disorder of fat metabolism) and chikungunya virus infections (spread by mosquitoes around the world).
So, there is a lot riding on AZD8601, Moderna's lead therapeutic asset—which is being co-developed with AstraZeneca under an agreement that dates back to 2013.
The mRNA therapy encodes the genetic recipe for making a growth factor, called VEGF-A, which helps promote blood vessel growth and is designed to regenerate damaged muscles in the heart.
Previously, scientists from AstraZeneca and Moderna, along with their academic collaborators, demonstrated that the treatment improved cardiac function following a heart attack in pigs, and that injections into the skin led to localized and temporary production of VEGF-A without severe side effects in people.
Now, a clinical team led by cardiac surgeon Vesa Anttila from Turku University Hospital in Finland has shown that injecting the mRNA directly into the sac surrounding the heart may be beneficial for people undergoing bypass surgery as well.
In the latest trial, seven participants received the active treatment and four got a placebo control. Although the study was likely too small to document statistically significant improvements in outcomes, the researchers did observe hints that AZD8601 improved heart-pumping capacity and reduced signs of heart failure.
Anttila presented the findings on November 15 at the Scientific Sessions annual meeting of the American Heart Association.
According to Zangi, the decision to focus on VEGF-A, rather than using mRNA to spur the production of some other heart regenerative factor, was largely an accident of history. Back when he started working on the project, in the early-2010s, it seemed like a good protein to prove the concept that mRNA-encoded therapeutics had potential.
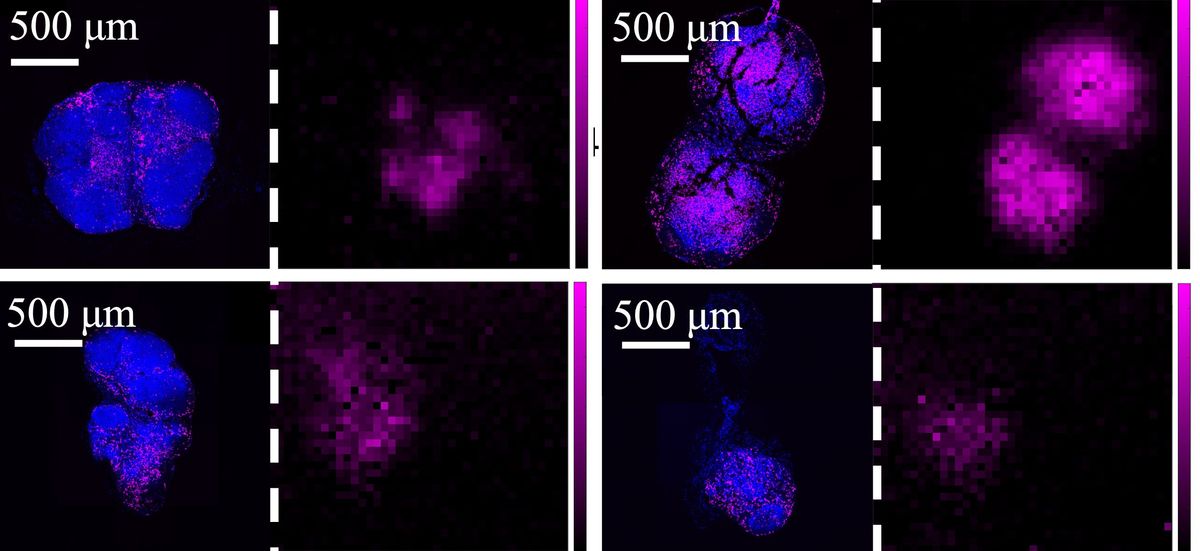
But since then, Zangi and his colleagues have identified several other proteins that, in mice at least, have far greater heart-healing effects when delivered via mRNA. In fact, Zangi has examined more than two dozen different genes and their encoded proteins as putative agents of heart regeneration. By his estimation, VEGF-A ranks near the bottom of the list in terms of its ability to restore cardiac function.
So, if AZD8601 is showing promise in patients, Zangi says, "one can only imagine what kind of an effect you'll have if you use the right gene."
Elie Dolgin is a science writer specializing in biomedical research and drug discovery. After a PhD spent studying the population genetics of nematodes, he swapped worms for words—entering journalism as an editor at The Scientist, Nature Medicine, and STAT. Now a freelancer, Elie is a frequent contributor to New Scientist, Nature, IEEE Spectrum, and more.