When a person’s heart is failing, water begins to build up in the lungs, making it increasingly difficult to breathe. The sensation, patients say, is like drowning.
Deciding whether it’s safe for that patient to go home can depend on whether the water level goes back down. But today the options for measuring lung water are cumbersome, such as taking chest X-rays, inserting a tube into the lung, doing blood tests, or even weighing the patient over time to quantify the decrease. The most hands-off method requires measuring the impedance of electricity passing through the patient’s body with a bulky vest, but this method can fail if the patient shifts position.
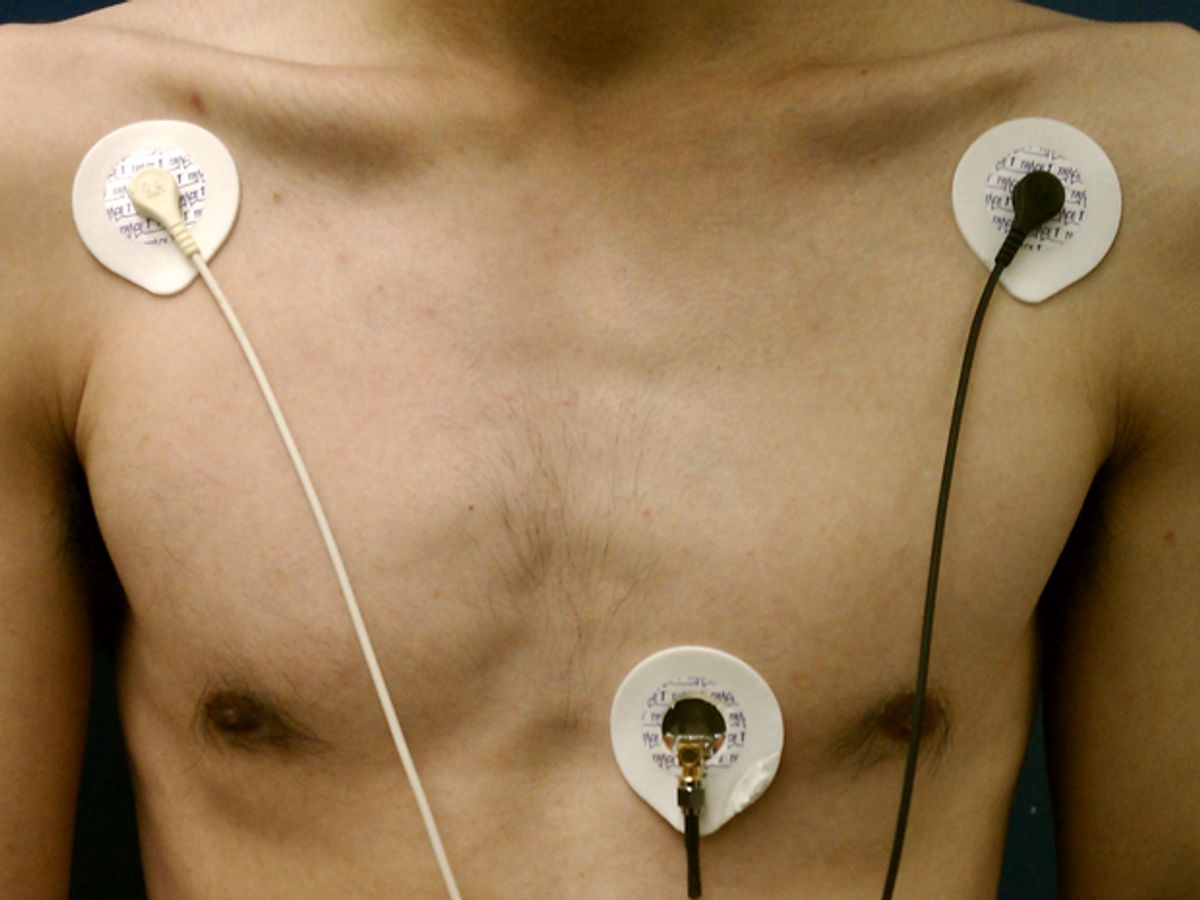
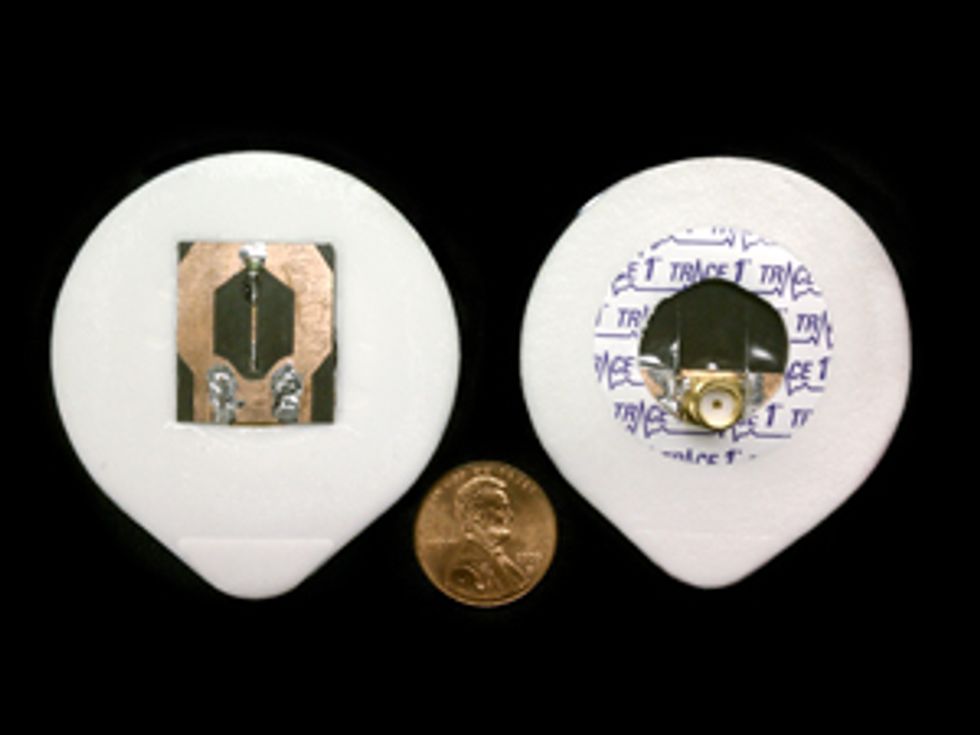
Now a team of researchers at the University of Hawaii, at Manoa, have a new way to measure lung water, along with many other vital signs. As their coin-size sensor rests on a patient’s chest, it emits microwaves and measures how they reflect. The list of what the researchers can decode from these patterns of reflected microwaves is only growing.
“Because of the ability for microwaves to penetrate the body, we can extract a wide variety of things, depending on what you are trying to monitor,” says Magdy Iskander, director of the Hawaii Center for Advanced Communications at the University of Hawaii’s College of Engineering. But the ability to measure fluid in a patient’s lungs might be what really sets the microwave stethoscope apart. The level of water in the lungs can be an indicator of a patient’s reaction to medication, the effectiveness of treatment for critically burned patients, and, most important, the extent of heart failure, he says.
To get a clear signal, Iskander’s team had to develop a compact microwave transmitter that beams tightly focused waves, something that ordinary antennas won’t do. “You can’t use microwave antennas—the signal is all over the place,” says Iskander. “What you receive next to it is coming from the transmitter and not from inside the body.” Instead, the device focuses the beams using waveguides. Upon capturing the reflected waves, the engineers apply advanced signal processing algorithms to pull out as much information as possible. The signals can then be sent to a smartphone or another display.
The group first tested the sensor solely for measuring lung water, but they soon realized that the data also revealed other vital signs—heart rate, breathing, and volume of blood pumped per beat. They’ve rigorously measured the lung water content of model systems and of animals and are just beginning human tests. In the meantime, the team has ensured that the stethoscope can accurately measure vital signs by using it side by side with a commercial set of medical sensors.
Ruthsenne Perron, a Ph.D. student who’s worked on developing the stethoscope’s different incarnations with Iskander, says that there are several devices for reading vital signs noninvasively. But their microwave stethoscope has a key difference—mobility. “We used some of the devices that they use in the hospital to benchmark our results,” she says. “But when the person is moving around, they just start beeping because they can’t handle the movement. That’s one of the advantages to what we have—it doesn’t hinder mobility for the patient.”
“It’s a huge challenge managing patients whose cardiac status varies a lot,” says John Spertus, a cardiologist at Saint Luke’s Mid America Heart Institute, in Kansas City, Mo. Spertus learned about the device in April and has helped Iskander’s group improve protocols for tests on humans. “The holy grail is to be able to detect early that somebody’s accumulating fluid,” Spertus says. Although there are other ways to approximate changes in lung water levels, he says, “none of them are either accurate enough or accessible enough in routine clinical care to reach the vast majority of heart failure patients. This is a really creative and novel solution for addressing that.” Still, Spertus acknowledges that the device needs more testing before it’s ready for hospital or home use.
According to Kenneth Foster, a professor of bioengineering at the University of Pennsylvania, in Philadelphia, it’s also challenging to ensure that new sensors will work with any kind of patient: “The device would need to give reliable and medically useful information for every patient who walks through the door—300-pound Sumo wrestlers to 95-pound cancer patients. It is premature at this point to speculate how the device will work in the real world of medicine.”
Brian Rosenfeld, vice president and chief medical officer of Philips Hospital to Home, says that a microwave stethoscope may be more practical for one-off uses than for full-time monitoring, which could add unnecessary expense to an intensive care unit. For continuous monitoring, as in a remote ICU, Rosenfeld thinks that physicians should instead use improved algorithms to collect and analyze the measurements already available, which would allow them to predict patient outcomes without extra equipment.
Besides beginning a human lung water-measurement trial at the Queen’s Medical Center, in Honolulu, Iskander’s group is considering other uses for the stethoscope—like sewing it into a shirt or a bra to monitor the medical condition of a soldier over time. The sensor could even watch for signs of dehydration, which earlier research has connected to lung water content.
“We’re just beginning to find out more about what our device can do,” says Perron.
About the Author
Sarah Lewin was an editorial intern at IEEE Spectrum from June to September 2014. A master’s student of journalism at New York University, she studied math at Brown University and enjoyed Spectrum’s tech-centric focus. Still, writing about the new microwave stethoscope was a challenge. “I had to carefully balance talking about the stethoscope’s technological potential with its applicability as a medical tool, which are two very different things,” she says. “It was troublesome, but rewarding.”
A correction to this article was made on 03 November 2014.