Genome sequencing is cheap, fast, and poised to revolutionize health care. In the one-hour radio special “Mapping Eliza: Decoding DNA Secrets,” IEEE Spectrum editor Eliza Strickland gets a glimpse of the medical future by getting her own genome sequenced. She takes listeners on her personal journey as she explores her genes, and investigates just how much they can reveal about her medical destiny.
This radio program is presented by PRX, the Public Radio Exchange, and received support from from the Alfred P. Sloan Foundation—enhancing public understanding of science, technology, and economic performance.

In this one-hour radio special, an IEEE Spectrum editor gets her genome sequenced and reveals her genetic destiny.
Transcripts
Jump to: Segment One | Segment Two | Segment Three
Segment One
Eliza Strickland: Have you ever lain awake in the middle of the night and wondered what will kill you in the end? I did a bit of that recently. I mentally scrolled through my family history and counted up the relatives who had died of heart disease—and then I vowed to go to the gym more often. I thought of an aunt who died of breast cancer and a grandfather who had kidney failure, and I sent internal messages to those body parts: How you doing in there? Stay strong. I need you!
I think most of us would agree that these kinds of midnight ruminations aren’t very useful. But what if there were a way to find out, with much more precision, what your biological weak points are? Would you want to know? And what would you do with that information?
I was lying in bed playing the mortality guessing game because the next morning I was flying to Texas to get all that precise information. In the name of journalism, science, and self-discovery, I’d had my genome sequenced. And I’m not talking about the mail-order genetic tests you can get from companies like 23andMe these days. Those companies send consumers a very limited set of results about their ancestry and possible health risks. I’m talking about a full, medical-grade genome scan that doctors interpreted for me.
I had given blood a few months before, and doctors at Baylor College of Medicine extracted my DNA and ran it through a cutting-edge genetic sequencing machine. The doctors analyzed the data, and I had to fly to Houston to get their predictions about my medical future.
JetBlue pilot: Ladies and gentlemen, JetBlue Airways welcomes you to Houston, Texas.
Eliza Strickland: But let’s leave me there on the runway for a minute. Before we go to Texas, let’s go to genetics class to talk over some of the basic science here. I’m lucky in that I have an on-call genetic tutor. Really, he’s on speed-dial, and I can go see him whenever I want.
Hi, Dad.
Sid Strickland: Hi, Little One.
Eliza Strickland: My father is a research scientist at Rockefeller University, in New York City, where he runs a lab that works on neurobiology and genetics.
Sid Strickland: We work on neuroscience, specifically on how things go wrong in neurological diseases. Our main focus these days is Alzheimer’s disease.
Eliza Strickland: He’s also really good at explaining science, which I’ve known since I was a little girl. So, Dad, let’s talk genetics. I inherited half of my DNA, my genetic material, from you, and half from Mom. And that combination produced the unique genome that is me.
Sid Strickland: Right. You can think of your genome as a set of encyclopedias that contain all the information about your biological makeup. Each of the volumes in that encyclopedia set is a chromosome—that’s a structure that packages your DNA and keeps it bundled up inside the cell. And if each encyclopedia volume is a chromosome, then all the topic articles in that book are the individual genes.
Eliza Strickland: So the topic articles in an encyclopedia explain things like giraffes and the primary exports of Ghana. What do the 20 000 or so genes in my genome do?
Sid Strickland: Well, the genes contain all the instructions for how to build proteins within your body, and those proteins carry on the business of living. For example, they’re the hemoglobin that carries oxygen through your blood, the enzymes that digest your food and contract your muscles, the antibodies that fight infections, the neurotransmitters that make things happen in your brain, they’re the…
Eliza Strickland: Okay, okay, I get the idea. Let’s take even a closer look at our genetic encyclopedia. If each of the topic articles is a gene, then you could say that the letters that spell out all the words in those articles are…
Sid Strickland: The letters of DNA. This part of our analogy works very well. All of our genetic information is encoded in a long molecule called DNA. That DNA is composed of a sequence of four chemicals that are actually called “letters,” because they’re referred to as A, T, C, and G. A complete human genome is made up of about 3 billion letters.
Eliza Strickland: So in each person’s genetic encyclopedia, the letters are in a slightly different order in some places, and that’s what makes us all unique individuals, right?
Sid Strickland: Exactly. The variation doesn’t just define the way you look—it doesn’t just explain the fact that you have your brown hair, your pretty blue eyes, and freckles. A harmful variant in your DNA can also directly cause a genetic disease or establish vulnerabilities to more complex diseases. No one thinks that your genome determines everything about your life—certainly your environment and your lifestyle choices play a role. But the genome, that’s what you start with.
Eliza Strickland: Okay, thanks. I think I’m ready to go to Texas.
JetBlue pilot: Ladies and gentlemen, JetBlue Airways welcomes you to Houston, Texas.
Eliza Strickland: Houston’s Baylor College of Medicine is a gracious but modern campus. Fountains and live oak trees decorate the open spaces between gleaming high-rises. It’s home to the Human Genome Sequencing Center, a leading institute for genetic medicine. Inside the labs, the researchers have ranks of bulky white machines that prepare DNA samples and sequence that DNA. It takes just a few hours for the newest machines to determine the sequence of 3 billion letters that makes up a person’s genome. And Baylor also has some of the best brains in the business.
James Lupski: I’m Jim Lupski. I’m professor and vice chair of molecular and human genetics and work also here in the Human Genome Sequencing Center.
Eliza Strickland: I sit down in a Baylor conference room with Lupski, who is a cheery, silver-haired physician. I’m honored that he agreed to scrutinize my genome. He’s been at the forefront of this genetic medicine revolution that’s been going on for the past few decades. Lupski was one of the hundreds of researchers who worked on the Human Genome Project, which produced a rough draft of the first complete human genome in the year 2000. That effort took more than a decade and cost more than US $3 billion in total. It was a pretty big deal. President Clinton called it…
Bill Clinton: …the most important, most wondrous map ever produced by humankind.
Eliza Strickland: That project sequenced a handful of people and combined their genetic information to produce a rough guide for what it means to be human. Then in 2007, Lupski helped reveal the first genome of a specific individual—that individual was Jim Watson, one of the founders of modern genetics. We’ll meet Watson later. And Lupski himself had his genome sequenced in 2010 to determine the genetic cause of a nerve disease that runs in his family.
James Lupski: I do have a neurologic disease, Charcot-Marie-Tooth disease neuropathy. I was quite excited when genomics had gotten to the level where we thought that we could try to apply it and figure out the disease in my very family. And so there was certainly personal curiosity in wanting to know, but it was a real problem too. So sequencing the genome and finding the cause of my disease was very gratifying for me.
Eliza Strickland: So Lupski knows what I’m going through as I settle into that Baylor conference room to talk through the results of my genetic sequencing. He can probably guess at the mix of nervousness and intense curiosity that I’m feeling. Will I learn something terrifying about my future, something that will change my whole life? Or will this be a major anticlimax? Lupski starts out by explaining that I’m an extremely unusual case for the Baylor team.
James Lupski: So the situation here is different from what we’ve usually done in the Whole Genome Laboratory, because there’s a specific clinical question.
Eliza Strickland: Most of the patients who get their genomes scanned are on what some doctors call “medical mystery tours.” That means their doctors don’t know the cause of their symptoms and hope that genome sequencing will provide answers. And some cancer patients are getting sequenced to let doctors personalize their treatment plans. And then there’s me. I’m one of only a handful of healthy people in the world who has gotten sequenced just because I’m curious—just to see what I can find out.
James Lupski: Here we have an individual, yourself, who’s normal. You don’t have any known health problems. And so we’re trying to look at your genome to see what variation might potentially have clinical significance.
Eliza Strickland: Lupski explains that the lab didn’t actually scan my entire genome. The machine didn’t sequence all 3 billion letters. Instead, it sequenced a portion of the genome known as the exome. The exome is all the parts of that long genetic sequence that actually contain the genes, which code for the creation of proteins.
James Lupski: The exome is the coding sequence of the genome. And currently it’s the information for which we have the most knowledge and understanding, that allows us some degree of interpretation. And that, believe it or not, encompasses less than 2 percent of the genome. So 98 percent of the genome we are not even looking at. And we don’t really know how to interpret a lot of that.
Eliza Strickland: All the rest of the genome, the other 98 percent, was historically dismissed as “junk DNA.” Researchers are now realizing that all that “junk” does play a role in human health, but the details aren’t yet clear.
James Lupski: So we’re still moving forward, and we still have a tremendous amount to learn. But that’s not to say we can’t already learn something from what we have.
Eliza Strickland: For now, Baylor’s lab specializes in exome scans. And they’re finding plenty within the exome to keep them busy.
James Lupski: We’re also learning that we all have many more genetic susceptibilities than we previously thought we had. And potentially, much of disease out there has a genetic influence.
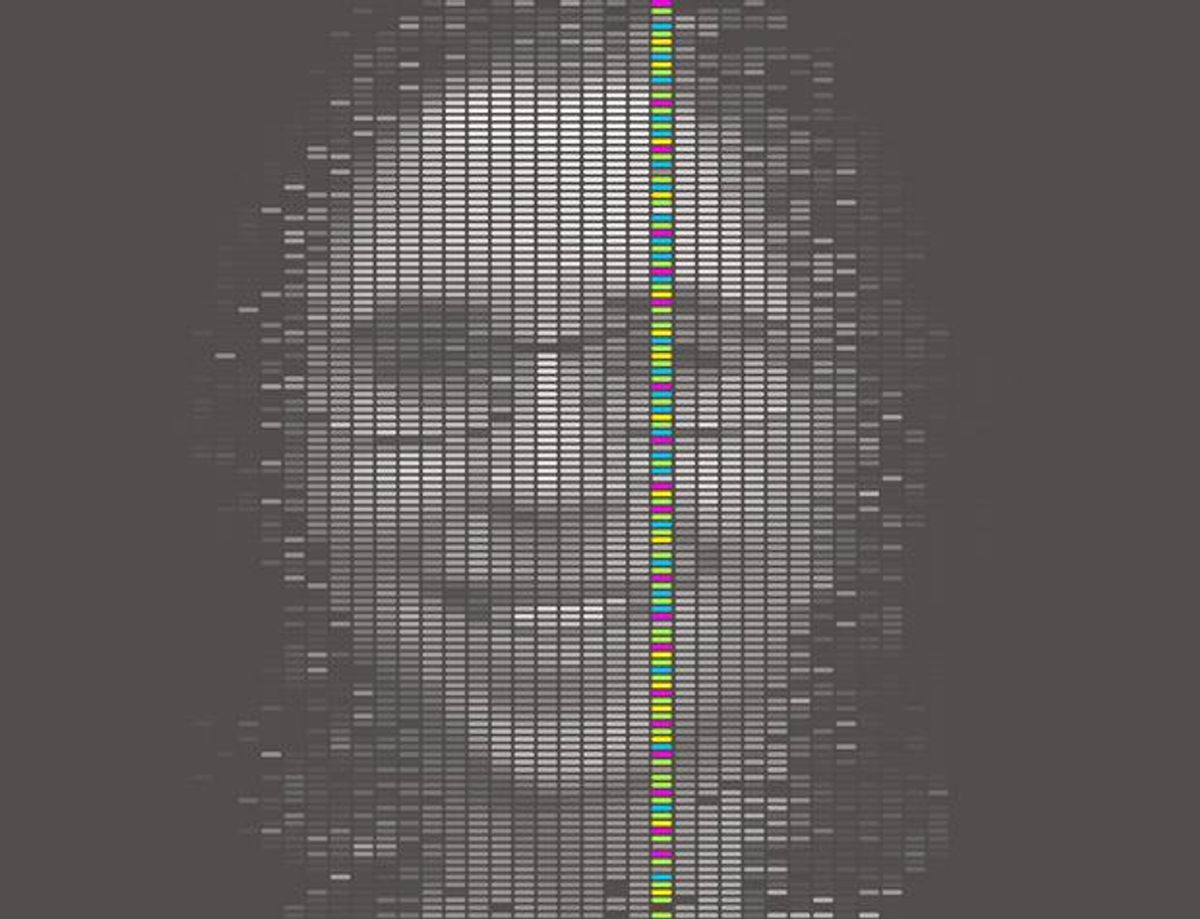
Eliza Strickland: So what did they look for in my genome? Also at the table is Christine Eng, director of Baylor’s Medical Genetics Laboratories. She’s holding a slim folder that I assume has my exome scan results in it. I’m having a hard time keeping my eyes off that folder. Finally, she slips out a six-page document and lays it on the table. It’s a six-page compendium of all my possible dooms. It’s everything the doctors found in my genome that could strike me down, or at least cause me a lot of medical unpleasantness.
Christine Eng: We are reporting things that, since you are a healthy individual, might affect you in the future. So these are adult-onset conditions for which you may not have a phenotype currently.
Eliza Strickland: That’s a doctor’s way of saying that I may not have symptoms for these diseases yet.
Christine Eng: We’re also reporting cancer predisposition genes, so again, where you would not have a phenotype currently but something that you might have to be on the lookout for in the future.
Eliza Strickland: Eng and Lupski think it’s only a matter of time before genome or exome scans become a routine part of medicine for healthy people like me, so we can all go through life knowing our vulnerabilities. In the medical checkup of the future, my doctor might take a family history and also order up an exome scan. All the genetic information could be put in my medical records. Then if my doctor sees that I have a particular vulnerability, he can advise me to take steps.
Christine Eng: So there might be instances where, perhaps, a patient might have to have more frequent screening by colonoscopy or mammography or some other modality because they know that they’re at risk for a certain condition. So there are definitely ways that you can approach either medical screening or other lifestyle changes if you know that you’re potentially at risk for something.
Eliza Strickland: So, I ask, What am I at risk for? Eng slides the report toward me. Some truly alarming words jump out.
Segment Two
Eliza Strickland: In a few minutes we’ll get back to my results and what I found out when I got doctors to decode my DNA. But first, let’s talk for a moment about the technology that enabled me to get my genome sequenced, because this is mighty impressive stuff. When the Human Genome Project finally finished sequencing the first human genome back in 2003, it had taken 13 years and cost about [US] $3 billion.
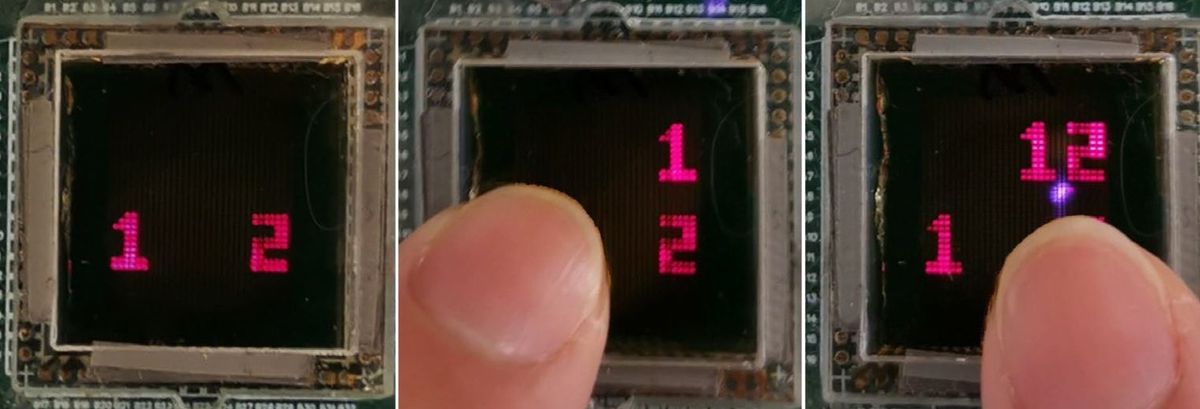
Several biotech companies now sell machines that can sequence an entire human genome in just a few hours. And one of those companies, Ion Torrent, says it will get the cost down this year to $1000 for a human genome. To learn more about how DNA sequencing is becoming almost affordable to consumers, I take a trip to an undistinguished office park in Guilford, Connecticut. I tromp past a pond full of geese to get to Ion Torrent’s headquarters. It’s a boxy building of black glass. Inside, I meet the company’s CEO.
Jonathan Rothberg: I’m Jonathan Rothberg. I’m the founder and CEO of Ion Torrent, which is a division of Life Technologies. My focus is on developing new technologies for decoding genomes and getting them out to the clinic and to researchers.
Eliza Strickland: Rothberg is a boisterous entrepreneur in his late 40s who flashes a boyish grin. And he doesn’t just express his exuberance by starting companies. Once he made his first millions in biotech, he built a life-sized replica of Stonehenge in his backyard, just for kicks. And he’s got plenty of other out-of-this-world ambitions.
Jonathan Rothberg: We’re literally sending a sequencing machine to Mars. We want to see if the code of life is there. And it’s not unreasonable to think that it would actually be DNA, because a huge amount of materials have gone between Mars and the Earth and the Earth and Mars when meteorites impact. So, yes, we are sending a sequencing machine to Mars.
Eliza Strickland: Rothberg is busy back here on Earth, too. He keeps shaking up genetic sequencing, because he keeps inventing machines that are faster and cheaper than everyone else’s. It was his idea to sequence the genome of the genetics pioneer Jim Watson back in 2007, and Baylor College of Medicine used his machines to do the job. He also collaborated with German scientists to sequence the genome of a Neanderthal, using DNA extracted from ancient bone fragments. Most recently, Rothberg invented a radical new sequencing machine called the Ion Proton. It combines basic chemistry tools with technologies from the computer industry, and that’s the machine the Baylor docs used to sequence my genome. In Ion Torrent’s Connecticut headquarters, Rothberg takes me on a tour of the labs.
Jonathan Rothberg: So, open laboratories. We always mix the disciplines. We literally have five disciplines that have come together to make this work.
Eliza Strickland: In the spacious main room, electrical engineers and biochemists work at desks side by side. The windows overlooking the duck pond are used as extra whiteboards, and they’re covered with scribbled diagrams of both circuit boards and molecules. In the labs, Ion Torrent’s newest machines are being tested.
Jonathan Rothberg: These are the Proton machines. So as I said, these machines are fully capable of enabling a $1000 genome. And right now they run two to four hours, but we’ve actually run runs as fast as 90 minutes, and we’re also speeding that up. So you have the scale, you have the simplicity, and you have the speed.
Eliza Strickland: Later, in a quiet conference room, Rothberg talks about how the machines work. The heart of the Ion Proton machine is a disposable chip about the size of a postage stamp. The chips are manufactured at a factory that usually makes microprocessors for the computer industry. Rothberg’s latest chip contains 165 million tiny wells, each of which holds one fragment of DNA. And at the bottom of each one of those wells is a sensor, which detects chemical changes to decode the sequence of that DNA fragment.
Jonathan Rothberg: So one piece of that DNA lands on each one of those sensors. Those sensors each then decode the order of those letters. So each one will decode 100 to 500 of those letters. That’s then put in a computer.
Eliza Strickland: Advances in computer processing make it possible to compare all these short sequences of letters and stitch them together into one long sequence of 3 billion letters: a human being’s genome. That genome can then be analyzed by experts, like my doctors at Baylor, to see what it says about that individual’s health. The part involving doctors is still time-consuming and expensive. But Rothberg says that with the sequencing itself getting so fast and cheap, it will soon be a routine part of health care. And he thinks that will revolutionize medicine.
Jonathan Rothberg: I do think genome sequencing is important. I do think it’s one of the four most important advancements in terms of health care. The first was clean water; the second was antibiotics; the third was imaging, like X-rays and MRI and CAT scan; and the fourth is sequencing. I’m seeing it change people’s lives. We’re seeing it unravel the mysteries of cancer and complex diseases.
Eliza Strickland: With the current top-of-the-line chip for Rothberg’s Ion Proton machine, it takes three chips to decode a whole human genome. But when he introduces his next chip, it will take just one. That’s when the price per genome will drop to $1000, he says. And that’s when it will start to make sense to use genome sequencing in hospitals and even doctors’ offices.
Jonathan Rothberg: But the important thing is, every year on average, within the United States, we spend about $6000 per person on health care. You can see it becomes pretty reasonable as part of health care to sequence a genome, or all of our genomes, when it’s a thousand, because it’s pretty easy to save a thousand bucks. If you give just one person the right cancer treatment, you can save $20 000. If you save a single day in the newborn intensive care unit, you can save tens of thousands of dollars. So I do see sequencing becoming a routine part of medicine over the next few years, first as part of cancer diagnostics and therapy, and then later as more general medical tests. So in the same way that you’ll have an X-ray, you’ll have your genome sequenced.
Eliza Strickland [voiceover]: I may be a pioneer in getting my exome sequenced. But it’s likely that many people—even some of you listeners—will follow in my footsteps. I think I should tell you what to expect if you get an exome report of your own. So what did I find out from my report?
Okay, prepare to get to know me really well, because genetic information is very personal stuff. Here are the most dangerous things that doctors found in my DNA. For starters, there’s Parkinson’s, the degenerative neurological disease that Michael J. Fox and Muhammad Ali suffer from. That possible killer comes from a suspicious mutation in my LRRK3 gene. Next…kidney failure: That possibility springs from a mutation in my ADAM19 gene. And there’s a mutation in my LMNA gene that raises a number of risks, including muscular dystrophy, cardiomyopathy, which is a weakening of the heart muscles, and a host of other obscure diseases.
But scary as all that sounds, none of these ailments are guaranteed to strike me down. While those genes have been linked to those diseases, my particular mutations to those genes haven’t been proven to cause so much as a tremor or an irregular heartbeat. So what does this report really give me? Red flags to watch out for. As I go through my life, I can be alert for symptoms that match those diseases.
Since genes are a family matter, I owe an explanation of my report to my parents and my sister. I have DNA from both my parents and share their mix of genes with my sister. Before I got sequenced, I talked the project over with all of them. I wanted to make sure they wouldn’t mind finding out about the Strickland family genome—and to make sure they were okay with me spilling our secrets on the radio. So when I get back from Houston with my results, I go over to my parents’ apartment in Manhattan to explain everything to my mom and dad.
Eliza Strickland: Hello!
Carol and Sid Strickland: Lizy! Hi, Lize!
Eliza Strickland: How are you? How’s it going?
Carol Strickland: How was your trip to Texas?
Eliza Strickland: Oh, it was fantastic.
Sid Strickland: We’re eager to hear about it. Come sit down.
Eliza Strickland: All right. Let’s get into this.
Eliza Strickland [voiceover]: We settled down around the dining room table to talk things through. My parents seem a little nervous and very curious.
Eliza Strickland: So, yeah. We are here to have a chat about the family genes and all the ways in which I inherited a little bit from column A and a little bit from column B. All right. So you guys ready to take a look and see what I found out?
Sid Strickland: Yeah, let’s have a look.
Carol Strickland: Okay.
Eliza Strickland: All right. I have the results right here. Let’s dig in. All right. So here we have my whole exome sequencing results. The first thing we’re going to look at is variants with previously reported disease association. So these are my genetic variants that could cause trouble. So it’s a very concise report. And the good news is that nothing is terrible.
Carol and Sid Strickland: Hooray! [ laughter]
Eliza Strickland: I mean, we’re all going to die of something eventually, but…
Sid Strickland: Well, that’s pretty bad.
Eliza Strickland: Did I bury the lead there? No, we’re all going to die of something eventually, but they can’t say exactly what. There’s no bizarre, terrifying, lurking medical skeletons in our family closet.
Carol Strickland: Very nice to know.
Eliza Strickland: What they did was they looked for genetic markers for adult-onset diseases and cancer predispositions. So the adult-onset stuff was interesting but totally unclear at this point in time. I think really what’s interesting is that it shows where genetic medicine is right now. It really clearly shows, I think, the promise and also the limitations of it.
Carol Strickland: But there must be proclivities which they identified, right?
Eliza Strickland: Yeah. Well, possible—possible susceptibilities.
Carol Strickland: Ah, okay.
Eliza Strickland: Yeah. So, like, they found a variant in this gene called the LMNA gene, which has to do with laminin—is that right?
Sid Strickland: Laminin?
Eliza Strickland: Laminin, yeah. But, you know, it’s a variant in the gene that is associated with a whole host of things that sound really bad, like muscular dystrophy, cardiomyopathy, which is, I guess, structural problems in the heart muscles.
Sid Strickland: The first one, laminin, is a—it’s a protein that’s outside the cell.
Eliza Strickland [voiceover]: It turned out my dad, the research scientist, knows all about laminin.
Sid Strickland: It’s kind of like the mortar in a brick wall, if you think of the bricks as cells and the stuff sticking them together. And that’s what this laminin stuff does. Therefore, it can affect a whole lot of different organs. That’s why I think they give you so many possibilities there. It can affect the kidney, liver, the brain, et cetera. And defects, real bad defects in this mortar between the cell, do lead to serious problems. But just a variant in this one laminin gene seems pretty unlikely to…
Carol Strickland: What does this mean? That there’s something wrong with your laminin production?
Eliza Strickland: It means that I have a variant in that gene, but they don’t know if my particular variant is causing me any significant problems.
Carol Strickland: Is a variant the same as a mutation?
Eliza Strickland: Yes. I am a mutant. [ laughter]
Carol Strickland: Oh, dear.
Eliza Strickland: And so are you, and so are we all.
Carol Strickland: I never suspected. So if you have this mutation, does that mean that you will develop one of these ailments at some point or not?
Eliza Strickland: No, it really does not signify that. It means I have a possible susceptibility to those diseases. Some people who have variants to this gene don’t have any symptoms of anything whatsoever. So it’s a variant that can be associated with disease but isn’t always.
Carol Strickland: So is there any intervention that they would recommend?
Eliza Strickland: For this, not really. The doctor said because this genetic variant has been associated with cardiomyopathy, with heart problems, in some cases, that it could conceivably make sense to do more heart monitoring as I age, to do EKG readings—eh, maybe.
Carol Strickland: My father, of course, had heart disease and died of a heart attack at age 67.
Eliza Strickland: Well, that’s—yeah, that’s the interesting thing, is the doctors I was talking with at Baylor didn’t really know my medical history. The things that they pulled out from my report were just variants that were scientifically provable. They were clearly there in my genetic code, but they didn’t know what they signified. So then as we talked, they said, “Well, does this mean anything to you? Like in the context of your family history, what do you think?” And so that was a very interesting part of the conversation.
And so another one, there’s a few more we can go into. There is a variant in the ADAM19 gene, which has been associated with renal failure, with kidney failure. And so I heard that and I thought, “Oh, well, my paternal grandfather did, in fact, have kidney failure at the end of his life.”
Sid Strickland: Right.
Eliza Strickland: Conceivably—conceivably this could be connected. So and that’s the kind of case where they said, “Well, you might in that case want to follow up with your doctors as the years go on.”
Eliza Strickland [voiceover]: We went through the rest of the report, including the Parkinson’s possibility and a bunch of other possible cancer and disease risks that are even more uncertain. By the time we get to the end of the report, my mom sounds both disappointed and relieved.
Carol Strickland: It doesn’t sound like it’s terribly predictive to me.
Eliza Strickland: At this point in time, no, it doesn’t seem terribly predictive.
Carol Strickland: Good, speaking as your mother.
Eliza Strickland: I guess I expected to find out more that seemed relevant to our family. What do you guys think? Does it seem like slim pickin’s to you?
Carol Strickland: Well, I think we got an A+. I’m happy.
Sid Strickland: Yeah, there’s nothing, as you pointed out, nothing catastrophic, nothing that’s a definite serious risk factor. That’s probably true for most people though.
Carol Strickland: So we’re both healthy, Sid and I. You’re healthy. Our other daughter is healthy. And, yeah, it seems like the absence of dramatic news is good news.
Eliza Strickland: I think this shows the state of genetic medicine. It doesn’t really make sense for a healthy person to run out and get their exome sequenced at this point in time, because you just don’t find out enough that’s medically actionable, as they say. But, you know, 10 years down the line, it might make sense.
Eliza Strickland [voiceover]: In the final analysis, my mom decides that the results show not just that I have a healthy exome, but that I have an excellent exome.
Carol Strickland: Well, we always felt you were an exemplary specimen.
Eliza Strickland: Thanks, Mom.
Sid Strickland: Specimen?
Eliza Strickland: I like it.
Carol Strickland: A paragon of virtue and wonder.
Eliza Strickland: That’s right. I have confirmed that I am a paragon of virtue and wonder by virtue of exome sequencing.
Eliza Strickland [voiceover]: A few days after that family chat, I go back to Connecticut to show my report to Jonathan Rothberg.
I tell him I hoped to get more definitive predictions about my medical future, but Rothberg says I got the best results possible for an early adopter.
Jonathan Rothberg: There’s two thing you’re observing. One is, because we’re at a tipping point and we’re just starting to sequence individuals, we don’t have a lot of information that correlates your sequence with either outcome or response to drugs. And so right now there’s literally only a handful of genes that we can tell you something about.
Eliza Strickland: It’s now fast and cheap and easy to sequence a genome. But understanding what all that information means for a person’s health is still really, really hard. Rothberg says we still have a long way to go with that analysis.
Jonathan Rothberg: But I think the first thing you have to realize is we are at an inflection point. There’s only a little bit of information. And that leads to the second point, which is it’s so important now to sequence tens of thousands of people, keep track of their medical records, so we can, if you will, annotate the rest of the genome. So five years from now, when somebody looks at their genome, you won’t get a little report. You’ll get a bigger report and you’ll get a report that has a lot more statistical significance because we’ll have studied hundreds of thousands of people.
Eliza Strickland: It takes me a while to digest everything that’s in my six-page exome report. Over the next few days, I Google the various rare and obscure diseases that I may be at risk for. And one of them stops me cold. As I read up on it, I realize that I have to have a serious talk with my mom about something she’s going to find unsettling. More to come, in a moment.
Segment Three
Eliza Strickland: I already told you about some of the scariest things I found out by getting my genome sequenced. My genes show that I have an elevated risk for Parkinson’s, kidney failure, and heart problems. These are problems that I don’t have any symptoms of now, at the age of 34. But they might strike later, and they could end me. But the report I got back from the doctors also includes genetic information about diseases that I’m likely a carrier for. To understand what that means, let’s have another lesson with the geneticist I have on speed-dial. Welcome back, Dad.
Sid Strickland: Hi again.
Eliza Strickland: Can we talk about my genetic inheritance? Tell me what I got from you and what I got from Mom.
Sid Strickland: You remember how we talked about your genome as a set of encyclopedias?
Eliza Strickland: Yeah, you said that each of my chromosomes is like a volume in that encyclopedia set. And I have 23 chromosomes, or volumes.
Sid Strickland: Actually, you have 46, because you have two copies of volume 1, two copies of volume 2, and so on. You got one complete set of encyclopedias from me, and one from Mom.
Eliza Strickland: So I’ve got two complete sets of encyclopedias—but they’re not identical. Because, obviously, you and mom are not identical, so neither is the genetic material you passed on to me.
Sid Strickland: Right. We talked before about the genes inside the chromosomes, which have all the instructions for keeping your body running. So you have two copies of each gene, and if they’re different, then you may have conflicting instructions.
Eliza Strickland: Geneticists talk about these genetic variants as being dominant or recessive. What do they mean by that?
Sid Strickland: If you’ve got a dominant version of a gene, that means its instructions override the instructions from the other version. The easiest way to understand this is to think about a gene that determines eye color. If you have one brown-eye version of the gene and one blue-eye version, you’re going to have brown eyes, because the brown-eye version is dominant, and the blue-eye version is recessive.
Eliza Strickland: So my blue eyes mean that I’ve got two copies of the recessive blue-eye gene, one from you and one from mom. And there was no brown-eye version to dominate?
Sid Strickland: Right, right. And it’s the same for lots of things—including some genetic diseases, like the lung disease cystic fibrosis, for example. If you have one copy of the gene version that causes cystic fibrosis, you’re okay, because your other copy of the gene, the normal copy, overrides it. In that case, doctors say you’re a carrier for the disease. But if you have two copies of the disease-causing version, then you actually have the disease.
Eliza Strickland: Okay, I get it. Thanks, Dad.
Sid Strickland: Sure thing, Little One.
Eliza Strickland [voiceover]: Luckily, there’s no cystic fibrosis in our family. But the genetic report I got back from the doctors does include a section about recessive diseases that I seem to be a carrier for.
To explore the details of my genetic report, I start googling all those recessive diseases. Here’s how one is listed: “Deafness, recessive. Usher syndrome. Gene CDH23.” When I read the list of symptoms associated with Usher syndrome, I stop short. It’s true that it’s most typically associated with deafness, and there’s none of that in my family. But it also causes problems in the inner ear that affect balance and can also damage the cells in the eye that allow us to see in the dark. That exactly describes the troubles my mom and her elder brother have been dealing with. So it’s time to head back to my parents’ apartment for a one-on-one chat with my mom. I settle down on a couch with my mom, and I take out my exome report again.
Eliza Strickland: So I wanted to come back and chat with you some more because I started delving more into the results.
Carol Strickland: Okay.
Eliza Strickland: And I guess at first I was focusing on, like, the things that might affect me later in life.
Carol Strickland: Yes.
Eliza Strickland: And I didn’t spend all that much time looking at the recessive stuff. These are things that I—that they say I’m likely a carrier for.
Carol Strickland: Right, because you got them from one of us, not both of us. Right?
Eliza Strickland: Right. Right. None of them had rung any alarm bells when I looked at them before.
Carol Strickland: Right.
Eliza Strickland: And they’re still not.…This isn’t superalarming, but it’s interesting, possibly illuminating.
Carol Strickland: Yeah, the deafness. I don’t know where in the world that came from, because I don’t know of any deafness in the family on either side.
Eliza Strickland: Yeah, I looked at that and I was like, well, that doesn’t apply to us. That’s nonsense.
Carol Strickland: You wouldn’t think so.
Eliza Strickland: I googled this.…It says here, you know, might be a carrier for a disease characterized by deafness, a disease called Usher syndrome. I was like, okay, well, I can look up Usher syndrome.
Carol Strickland: Right. Is that rather dire?
Eliza Strickland: It’s not—well, it’s dire in some forms, definitely not in the form that has to do with us. So Usher syndrome is characterized by problems with the inner ear.
Carol Strickland: You’re kidding.
Eliza Strickland: And also by night blindness.
Carol Strickland: Oh, my gosh. I’ve got that.
Eliza Strickland: Yeah.
Carol Strickland: And my brother too. Oh, no. Okay. I’m so glad to find out.
Eliza Strickland: Isn’t that interesting?
Carol Strickland: Yes. I will google it myself.
Eliza Strickland: Yeah, so I mean, I was just looking at the characteristics, and I was like, well, that’s Mom and Uncle John.
Carol Strickland: It surely is.
Eliza Strickland: And so, yeah. So…
Carol Strickland: I have a syndrome! Okay. Okay. I can deal with it.
Eliza Strickland: Yeah. So, I mean, it’s, you know, it’s not certain, but it seems quite likely.
Eliza Strickland [voiceover]: I asked my mom to talk a little bit about her symptoms.
Carol Strickland: Well, the night blindness has been going on for as long as I know. I remember the first time I ever tried to develop a photograph in a dark room, and Dad was quite light-adjusted to it, and he could tell what was in the developing tray, but I couldn’t. I couldn’t see a thing. So I was just kind of dabbing around at things, not knowing if I was dabbing at the photograph in the developing tray or not. And that’s when he said, “Oh, my God. You can’t see in the dark.”
Eliza Strickland [voiceover]: My mom says her vision problems haven’t gotten worse, but her balance problems have.
Carol Strickland: But, okay, so the balance problem has been getting worse and worse for the last few years. And at first it was just kind of tottering around and, you know, not staggering exactly, but being very tippy. And now, you know, just walking, it’s not exactly a struggle, but I’ve got to concentrate to keep upright. And so that has been progressively getting worse. And my brother, oh, really, he’s awful now.
Eliza Strickland [voiceover]: My mom never imagined that her vision and balance problems might be connected. I tell her she’d have to get a genetic test for Usher syndrome to find out for sure if that’s the correct diagnosis. Then she asks the inevitable question: If it is the right diagnosis…?
Carol Strickland: So is there anything to do?
Eliza Strickland [voiceover]: I have to tell her: No, not really. There’s no cure for Usher syndrome. For now, her only option is to be monitored for further vision loss. And physical therapy might help her balance problems.
Eliza Strickland: I think you’re at the frontier of genetic medicine right here.
Carol Strickland: Okay.
Eliza Strickland: It’s very rare that the patient can come in to the doctor saying, “I know about my genes.”
Carol Strickland: That’s right.
Eliza Strickland: “And now you have to build your treatment plan around my genetic knowledge.”
Eliza Strickland [voiceover]: My mom’s situation really shows the conundrum of genetic medicine right now. Doctors are getting better and better at using genome scans to diagnose problems. But that doesn’t mean they can suggest any helpful treatment. That’s why some high-profile geneticists think that genome scans just aren’t very useful yet. One of those skeptics is none other than the genetics pioneer James Watson. He and his colleague Francis Crick started the genetics revolution back in 1953. They figured out the double-helix structure of the DNA molecule and realized that it encoded all the instructions for life in a long sequence of chemicals. Ever since then, Watson has watched the progress of the revolution that he began. And that revolution touched his own life in 2007, when he became the first human being to get his own personal genome scanned. So you’d think he’d be more…enthusiastic.
So I take the train to Cold Spring Harbor Laboratory, on Long Island, to meet Watson. Cold Spring Harbor Lab is a picturesque little campus on the shore of Long Island Sound, but it’s a world-class center for genetics research. Watson is in his eighties now, and his title at the lab is “chancellor emeritus,” but he still goes to his wood-paneled office most days. That’s where I met him.
James Watson: I’m Jim Watson. I’ve been at the Cold Spring Harbor Lab for 45 years. I had my DNA sequenced in 2007 or something like that.
Eliza Strickland: On his desk sits a heavy gold medal: That’s the Nobel Prize for medicine that Watson won in 1962 for discovering DNA’s structure. That discovery led to all the marvels we’ve talked about in this show, including the sequencing machines that are making genome scans so fast and cheap. Watson himself got sequenced because of Jonathan Rothberg, who we met earlier in the show. Rothberg, the inventor of some of those sequencing machines, asked to scan Watson’s genome.
James Watson: He must have been persuasive. I think at the time I’m not sure I believed it was actually, you know, going to happen. But I gave the blood sample and didn’t think about it until they told me they’d actually started sequencing.
Eliza Strickland: Even though Watson was the first human being to get a full report of what’s in his personal and unique genome, he hasn’t delved much into the results.
Jim Watson: And I showed probably almost a pathological lack of interest in my own sequence.
Eliza Strickland: Watson did ask the doctors to edit out one part of his genome report.
James Watson: I didn’t want to know whether I had any risk to Alzheimer’s. Because, you know, without fearing it, you know, I just figure I have such a short time to do everything I’m trying to do now, so I’ll be lucky to finish things I’ve started before I’m really too old.
Eliza Strickland: So you felt that if you knew your Alzheimer’s risk it would just worry you all the time?
James Watson: Yes.
Eliza Strickland: These questions of privacy and ethics will keep coming up as more and more people get sequenced: How much bad news do we want to get about our futures? If a doctor finds something scary in a patient’s genome, does he have an obligation to tell the patient? Despite all of Watson’s reservations, he admits that he did get one useful piece of medical information out of his sequence. He found out that his body doesn’t handle drugs called beta blockers very well. And he was taking them to control his blood pressure.
James Watson: I turned out to be a poor metabolizer.
Eliza Strickland [voiceover]: That was useful information, Watson says, and he changed his medication plan. But he doesn’t think that proves the usefulness of genome scans for everyone.
Eliza Strickland: So take someone like me. I’m relatively young; I’m 34. I’m relatively healthy.
James Watson: Yes.
Eliza Strickland: Would you advise someone like me to go and get their genome sequenced if it was cheap enough and easy enough?
James Watson: No.
Eliza Strickland: Why is that?
James Watson: Unless you have a real perceived need, don’t sequence yourself before you’re 80, because I think, just some people, it won’t matter, but others will, you know, learn something and just worry the rest of their lives thinking they have some inherent defect, which could set them back. And so I don’t know how to prevent that.
Eliza Strickland: Watson worries that the companies that build the machines and the hospitals that offer the genome scans are mostly interested in making money on these tests.
James Watson: We can produce more data now than we have people or, you could say, time, to interpret it, and I’m just afraid we’re—just because sequencing will make money and everything, and people want to sell machines, that we may be having the sequencing run ahead of our ability to get our money’s worth.
Eliza Strickland: Watson thinks that targeted genetic testing will be good enough for most people. That means if a patient has some symptom, he can get checked for a few specific genetic mutations based on his doctor’s best guess of what’s wrong. Whole genome scans, Watson thinks, may just raise troubling questions.
James Watson: And so what if you’re looking at your sequence, you discover that you have two mutations in these disease-provoking genes, but they haven’t even been seen before. So should you worry or not? And I would say the answer is certainly don’t worry, because probably they’re not the cause. If you think yourself normal, continue to consider yourself normal.
Eliza Strickland: So at the end of my genomic adventure, do I consider myself normal? Now that I’ve got a six-page report that lists all the ways my body may break down and fail me, how do I carry on?
To try to make sense of all this, I do what I typically do. I sit down with my husband, Chris, and we talk it all over.
So, hello, darling.
Chris Thompson: Hi, baby.
Eliza Strickland: He wants to know what I got out of this whole experience.
Chris Thompson: Well, I guess I wonder if there is, in fact, any medical pragmatism to understanding your exome at this point. Or if, in fact, it’s just a sort of very expensive way of fantasizing about how you’re going to die in some sort of romantic gothic sense.
Eliza Strickland: That’s a great summation. No, I think it is just barely medically useful at this point in time. I think if I started to show symptoms associated with kidney disease down the road, then it would be useful to have this knowledge and say, oh, well, this is the particular genetic variant I have that’s associated with this particular kind of kidney disease and kidney failure; let’s look into that. But I don’t think it makes sense for me to run into the doctor’s office and brandish this report and say, like, check me for everything.
Chris Thompson: That said, are you happy you did it? Do you recommend it?
Eliza Strickland: I guess that’s two different questions. Yeah, I’m happy I did it because I am a curious person and this was a fantastic opportunity to gratify my curiosity. So I’m happy I got it done, but I wouldn’t recommend it necessarily to healthy people.
Chris Thompson: Why? I was wondering about that. Why do you think that people who are sick ought to have it, have their exome diagnosed, as opposed to anybody else?
Eliza Strickland: Well, at this point in time, there’s still a significant cost factor. To get your exome sequenced in a medical lab costs about 7000 bucks these days, and that’s a significant amount of money. And insurance companies would only pay for that if there was some reason to be looking into your exome. If a healthy patient wanted to get their exome sequenced, they’d have to pay out of pocket probably. And there just aren’t enough medically actionable results at this point in time to make that worthwhile. But for certain types of sick patients, I think it already makes sense, and I think it’ll make sense for a broader and broader spectrum of sick people as time goes on.
Chris Thompson: I wonder what it felt like to be presented with a certain kind of mathematical or scientific precision the odds that you’re going to die in the following ways. I’m just wondering how you felt about that and whether you think it was worth it, or how you steeled yourself for that kind of revelation.
Eliza Strickland: I think that’s a, yeah, it’s an interesting question. And sort of by coincidence, I’m reading this book at this point in time called Manalive, which is a great book by G.K. Chesterton. So the book features this character, Innocent Smith, who runs around England brandishing a revolver, and whenever he finds a pessimist or a cynic or someone who thinks that life isn’t worth living, he threatens to shoot them. So he uses death as a reminder to live life to the fullest. So you could see this as a similar situation, in which you’re confronted with your own mortality. You have to think about how you live your life and how to make the most of it. And I actually like that reminder. I don’t mind it at all.
Chris Thompson: Well, I’m glad to learn that you’re not going to die of anything any time soon.
Eliza Strickland: That we know of. I mean, there’s a lot of buses out there on New York City streets. I could be hit by one any minute.
Chris Thompson: It’s not in your exome.
Eliza Strickland: I don’t have the bus gene?
Eliza Strickland: You’ve been listening to “Mapping Eliza: Decoding DNA Secrets,” a production of IEEE Spectrum magazine. For related stories and more information, check out the IEEE Spectrum website: Spectrum.ieee.org. We had support for this program from the Alfred P. Sloan Foundation—enhancing public understanding of science, technology, and economic performance. There is more information on Sloan at Sloan.org.
Our thanks to Susan Hassler, Glenn Zorpette, John Barth, and my very patient family. Also, Paul Ruest at the Argot Studio. Our technical producer, Dennis Foley, mixed the show and also recorded on-site in Texas. Our executive producer is Sharon Basco. I’m Eliza Strickland. This program is presented by PRX, the Public Radio Exchange.