THE INSTITUTE In severe cases of COVID-19, the virus causes respiratory distress, making it difficult for patients to breathe. Pulmonary therapy, such as deep breathing exercises, can help prevent severe respiratory complications, according to the American Lung Association.
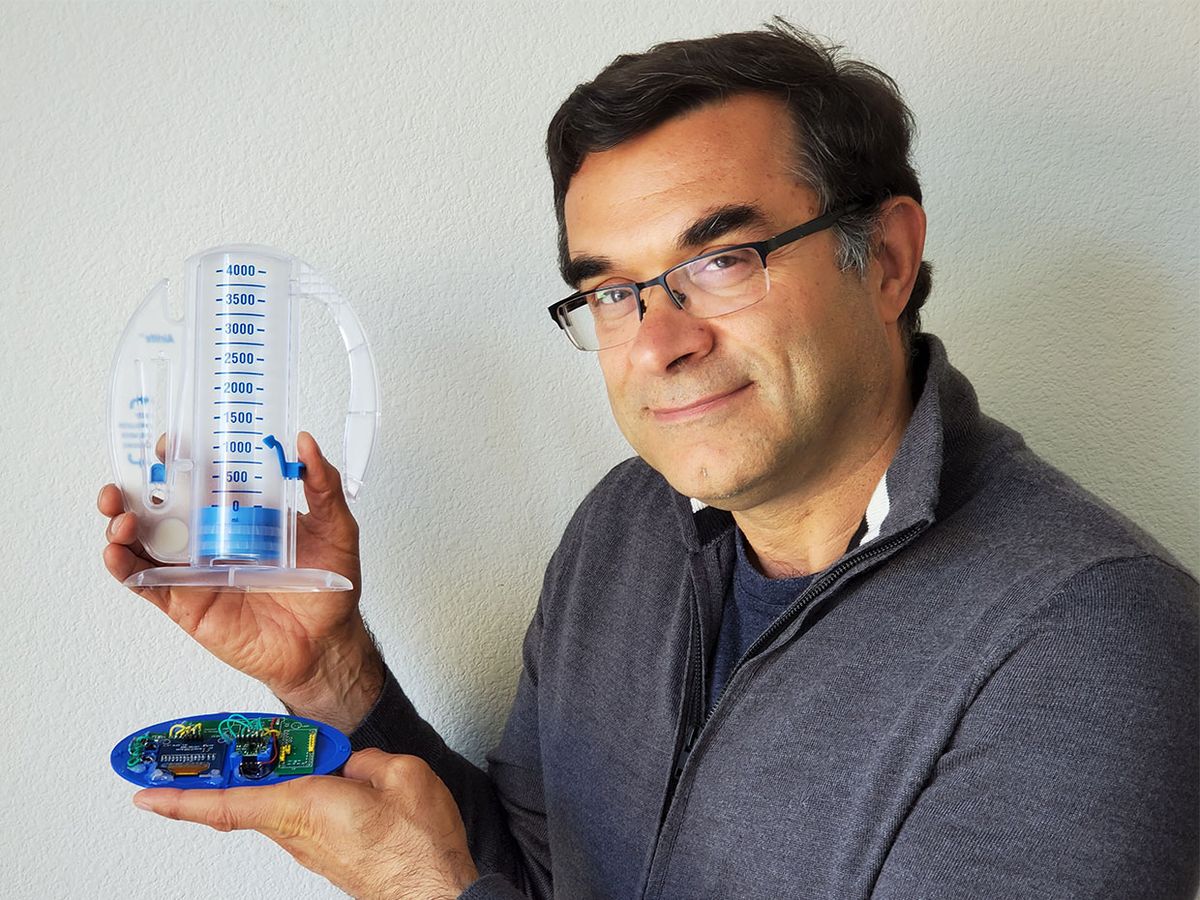
The Advanced Internet Technologies in the Interests of Society Laboratory—a research lab at Sonoma State University in Rohnert Park, Calif., has developed InSee, an auxiliary device that attaches to an incentive spirometer. Incentive spirometers are medical devices that are used to help patients improve the functioning of their lungs by measuring the patients’ air volume as they inhale and exhale into the device. InSee can also remind patients to use the spirometer, monitor how often they use it, and record how well they perform.
IEEE Member Farid Farahmand is the director of the lab, which develops Internet-based technology solutions for educational, environmental, and healthcare problems.
The Institute asked Farahmand about InSee.
This interview has been edited and condensed for clarity.
What problem are you trying to solve?
COVID-19 patients are often bedbound, which limits their daily movement and often results in minimal lung expansion. This can lead to severe pneumonia, acute respiratory distress syndrome, and mechanical ventilation, which may result in the death of the patient.
Incentive spirometry is a standard practice in postoperative care and has been proven to help patients improve their lung function, but its main drawback is patient compliance. Healthcare providers train patients how to use the device, but they are not able to monitor the patients’ progress.
What technologies are you using?
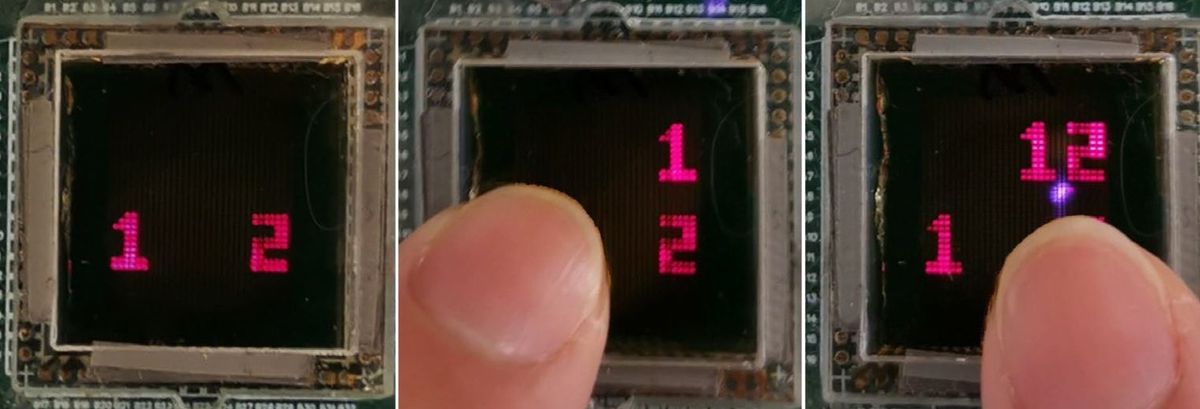
InSee uses an infrared sensor, which monitors the movement of the spirometer’s internal cylinder [Editor’s note: the cylinder contains a piston whose movement measures the volume of air that is inhaled]. Using time-of-flight calculations, cylinder movement is converted to tidal volume, which is the volume of air moved with each breath and a key marker of respiratory function.
The data the device collects is stored and accessed remotely on a computer through WiFi.
Explain how your project works.
Using InSee, a doctor sets a target tidal volume for the patient before use. While sitting upright, the patient puts the mouthpiece [of the incentive spirometer] in his mouth and closes his lips tightly around it. He slowly exhales and inhales as deeply as he can. The patient must breathe through his mouth or else the device won’t work.
[The incentive spirometer contains two chambers. The first, located in the center of the device, measures the volume of the patient's breath. As the patient inhales, a piston moves along a numbered grid, marking the air volume. A second chamber beside the first measures the speed of the patient's breath.]
As the patient uses the device, InSee measures the tidal volume and determines how many times a patient failed to reach the target tidal volume. It also determines the maximum tidal volume the patient was able to reach and how long it took the patient to reach a specific tidal volume.
Using a red blinking light, InSee automatically reminds the patient to use the device at the frequency set by the doctor. The only way to shut off the light is by using the spirometer and reaching the target tidal volume.
What challenges have you faced and how did you overcome them?
Packaging the device was very challenging. There is a wide variety of disposable incentive spirometers available to medical facilities. We designed InSee to fit those that are most often used in hospitals, such as the Vytaire Medical AirLife Volumetric Incentive Spirometer. This allows InSee to easily and readily fit a variety of low-cost disposable incentive spirometer without any modifications.
What is the potential impact of the technology?
By adding InSee to existing incentive spirometers, hospitals will be able to record, monitor, and evaluate patient’s respiratory exercises as well as remind and encourage the patient to use the device if InSee detects a low level of activity.
This will also minimize contact between patients and providers and reduce the risk of transmission of the coronavirus.
How close are you to the final product?
We were granted a U.S. patent in April and hope to receive funding soon so we can build 200 units and begin clinical trials. Trials will take place at HCA Gulf Coast Hospital in Houston and Houston Methodist Hospital, pending approval from the Institutional Review Board.
How can other IEEE members get involved?
Members who are interested in helping us improve the electrical and mechanical design of our device can email me.
Attention IEEE members: are you part of a team responding to the COVID-19 crisis? We want to hear from you! Wherever you are and whatever you are doing, if you are helping deal with the outbreak in some way, let us know. Send us accounts of anywhere from 200 to 800 words, or simply give us a rough idea of what you are doing and your contact information. Write to: k.pretz@ieee.org
This article appears in the December 2020 print issue as “Smart Device Helps Monitor COVID-19 Patients’ Breathing.”
IEEE membership offers a wide range of benefits and opportunities for those who share a common interest in technology. If you are not already a member, consider joining IEEE and becoming part of a worldwide network of more than 400,000 students and professionals.