Months into the COVID-19 pandemic, the United States has finally moved from relying entirely on a single, flawed diagnostic test to having what may soon be an onslaught of testing options available from private entities. The U.S. Food and Drug Administration over the last three weeks has authorized the emergency use of more than 20 diagnostic tests for the novel coronavirus known as SARS-CoV-2.
Those add to the hundreds of tests that researchers are developing globally. The Foundation for Innovative New Diagnostics (FIND) in Geneva, Switzerland keeps a running global list of COVID-19 tests that, as of 3 April, neared 400.
To help our readers sort through the deluge of diagnostics, here, we provide a simple explainer on coronavirus testing.
What kinds of tests are used to confirm COVID-19?
Diagnostics for COVID-19 typically fall into two broad categories: tests that detect proteins associated with the virus, known as immunoassays, and tests that detect the virus's genetic code, known as nucleic acid or molecular tests.
Nucleic acid-based tests are the most sensitive in early detection of infection, and have been widely used during the COVID-19 pandemic. These tests typically rely on a decades-old technique called reverse transcription polymerase chain reaction, or RT-PCR.
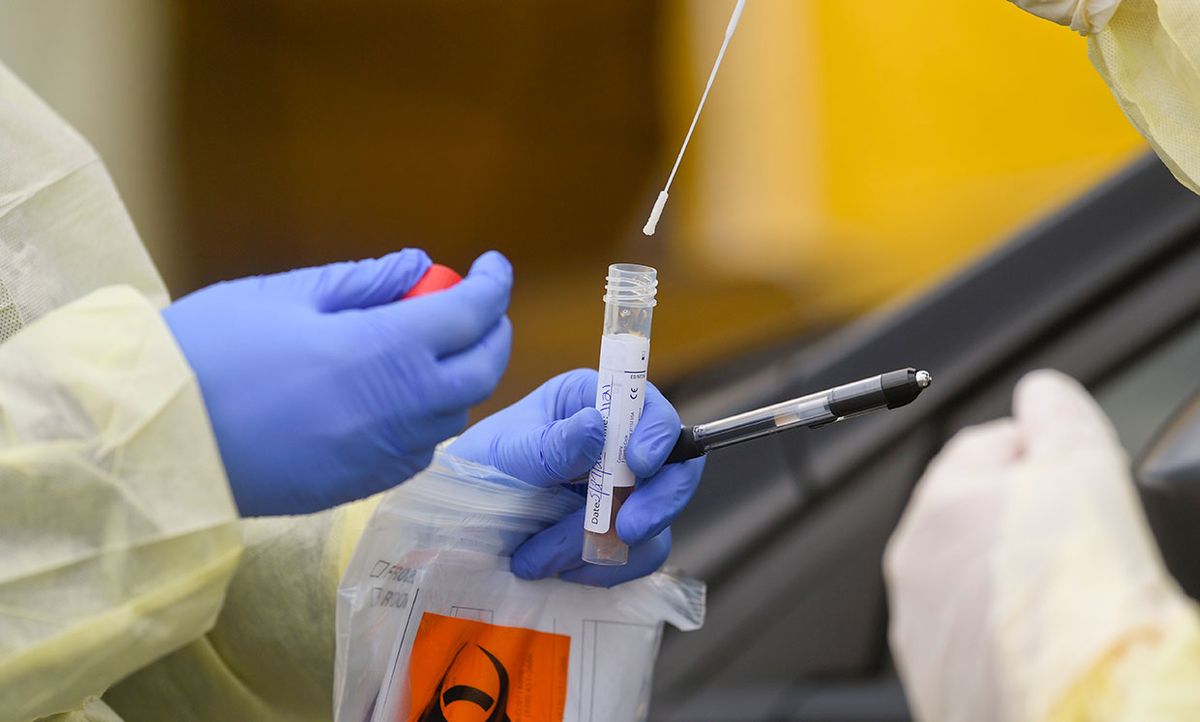
First a sample is taken by swabbing the nasal passages or throat. To find evidence of the virus, researchers use PCR to copy and amplify any segments of viral genetic code found in the sample, which makes it easier to detect. This typically involves adding reagents and enzymes, and raising and lowering the temperature of the mixture, known as thermal cycling.
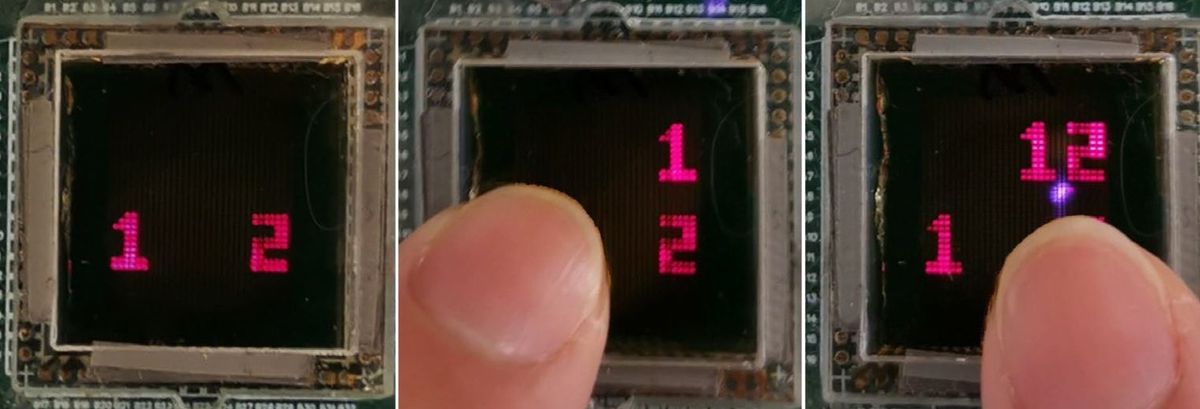
Software then determines when the number of copies of the target sequence exceeds a threshold, indicating if the novel coronavirus is present, and at what concentration. (Scientists have known and tracked changes in the virus's genetic code for several months. This information has enabled scientists to develop the necessary components for PCR analysis.)
PCR is the gold standard in viral diagnostics. “Because the sensitivity is so good, it should be the best mechanism for picking up copies of the virus at very early stages of infections," says Paul Yager, a bioengineer focused on the development of diagnostics at the University of Washington in Seattle. “Even if someone is asymptomatic—not yet showing fever or cough—you might very well still pick up a positive."
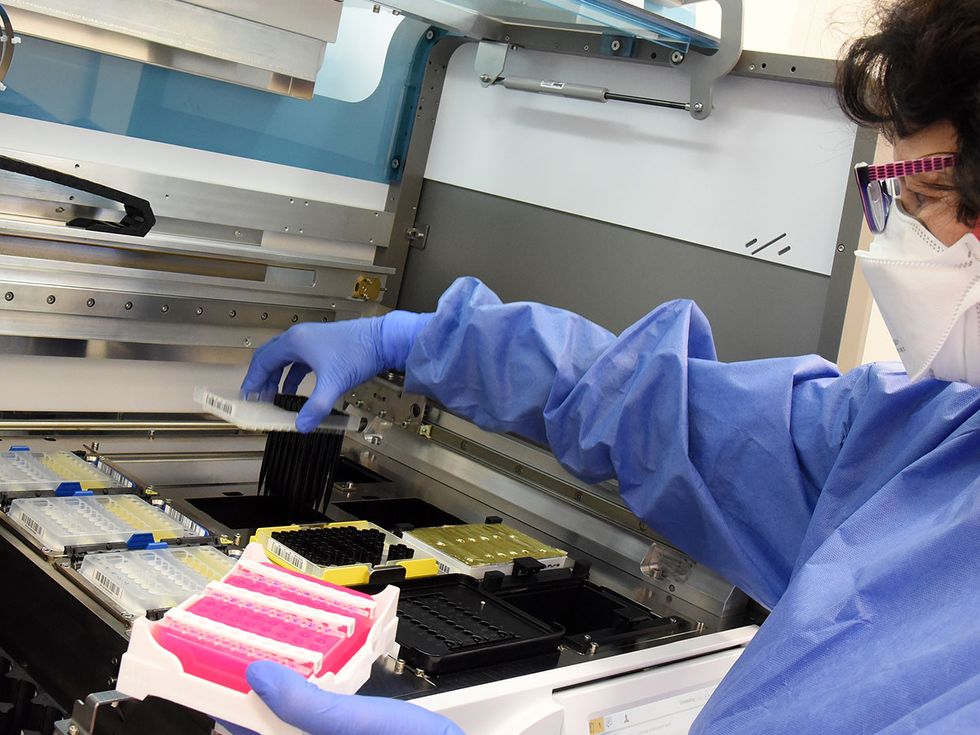
Diagnostic developers and labs around the world have customized their PCR tests to detect the novel coronavirus. Many of the available thermal cycler machines reside in large centralized laboratories that accept samples by mail. Results can take days due to the logistics of getting the sample to the lab.
Some hospitals and other health care settings, and research labs, have machines on site capable of PCR analysis. These devices can provide results in a couple of hours or less. The newest nucleic acid tests can produce results in minutes. Some of these are being customized to detect SARS-CoV-2.
For example, health giant Abbott has a device called ID NOW, introduced in 2014, that's the size of a toaster and provides flu, strep, and respiratory syncytial virus test results in minutes. Last month, the company quickly put together an assay for COVID-19 testing that is compatible with its ID NOW platform. Positive results can be ready in five minutes, according to the company.
Abbott on 27 March announced that it had received for this device an Emergency Use Authorization from the FDA—a green light to market the test during the current public health emergency. The company will be making the tests available this week to urgent care settings in the United States, where the majority of ID NOW instruments are in use, the company says.
What are immunoassays?

The other primary way to test for COVID-19 is with an immunoassay. Rather than analyzing genetic material, these tests detect proteins produced either by the virus itself, or by the body's immune system in response to the virus. The tests can detect evidence of past or current infections.
Viruses are covered in protein structures, called spikes, that are unique to that virus. As the body's immune system kicks into gear to fight the infection, it produces its own unique proteins, called antibodies, that attach to the protein structures on the virus.
The unique linkage between antibodies and their respective viral proteins, or antigens, makes both parties good targets for diagnostics. Immunoassays take advantage of this. Such tests use antibodies and antigens as bait to capture their respective partners.
A sample—typically blood, plasma, or serum—is run through the test, usually in the format of a lateral flow assay. Antibodies in the blood sample will recognize and bind with the antigens on the test. Likewise, viral antigens in the blood sample will bind with the antibodies on the test. Any binding that takes place indicates a positive result.
Immunoassays aren't as sensitive as nucleic acid tests in the earliest days of an infection. “The challenge is you need an awful lot of virus to see a signal," says Yager. But immunoassays tend to be easier to use, portable, and fast—important features for use in a busy emergency department. Rapid tests are particularly useful as triage tools, in that they can quickly tell health care workers whether a patient should go to the quarantined part of the hospital, or the regular part of the hospital.
Some types of immunoassays, called serological assays, can be used weeks after an infection to confirm that a person had the virus and recovered. These are in development for coronavirus. For example, the University of Minnesota and the Mayo Clinic say they are readying such a test, which could be helpful in determining which health care workers have immunity.
So far, all of the COVID-19 diagnostics that have received the FDA's Emergency Use Authorization have been nucleic acid-based tests. But many immunoassays are in the pipeline. Nearly half of the tests on FIND's global list of COVID-19 tests in development are immunoassays.
What does not exist is an at-home, sensitive, disposable test for COVID-19, similar to a pregnancy test. “There's virtually nothing" like that for COVID-19, says Yager. In fact, the FDA on 20 March warned of “unauthorized, fraudulent test kits that are being marketed to test for COVID-19 in the home."
The FDA's warning, along with updates to its policy, stymied development of at-home sample collection kits as well. These kits provide sample collection equipment so that people can swab themselves at home and send the sample into laboratories for analysis. Several companies developing such kits reported putting that work on hold, after the warning and further guidance from the FDA.
Emily Waltz is a features editor at Spectrum covering power and energy. Prior to joining the staff in January 2024, Emily spent 18 years as a freelance journalist covering biotechnology, primarily for the Nature research journals and Spectrum. Her work has also appeared in Scientific American, Discover, Outside, and the New York Times. Emily has a master's degree from Columbia University Graduate School of Journalism and an undergraduate degree from Vanderbilt University. With every word she writes, Emily strives to say something true and useful. She posts on Twitter/X @EmWaltz and her portfolio can be found on her website.