Startup T2 Biosystems in Lexington, Mass., got the U.S. Food and Drug Administration's (FDA’s) nod on Monday for a device that quickly and accurately detects dangerous pathogens. The instrument is based on miniaturized nuclear magnetic resonance (NMR) technology developed by MIT and Harvard Medical School researchers who founded the company eight years ago. The Harvard researchers are also developing the tool for cancer detection.
Today’s culture-based diagnostic tests for viral and bacterial infections are expensive, and require a few days wait, even with the equipment at full-scale laboratories. A speedy, portable, sensitive detector could save lives and money.
T2 Biosystem’s fully automated bench-top tool delivers results in three to five hours and is more sensitive than culture-based tests, according to the company. It works like this: A clinician loads a patient’s blood sample into a disposable test cartridge containing a few reagents, inserts the cartridge into the machine, and waits. The machine is capable of detecting a range of biological material including proteins, DNA, small molecules, viruses, and bacteria.
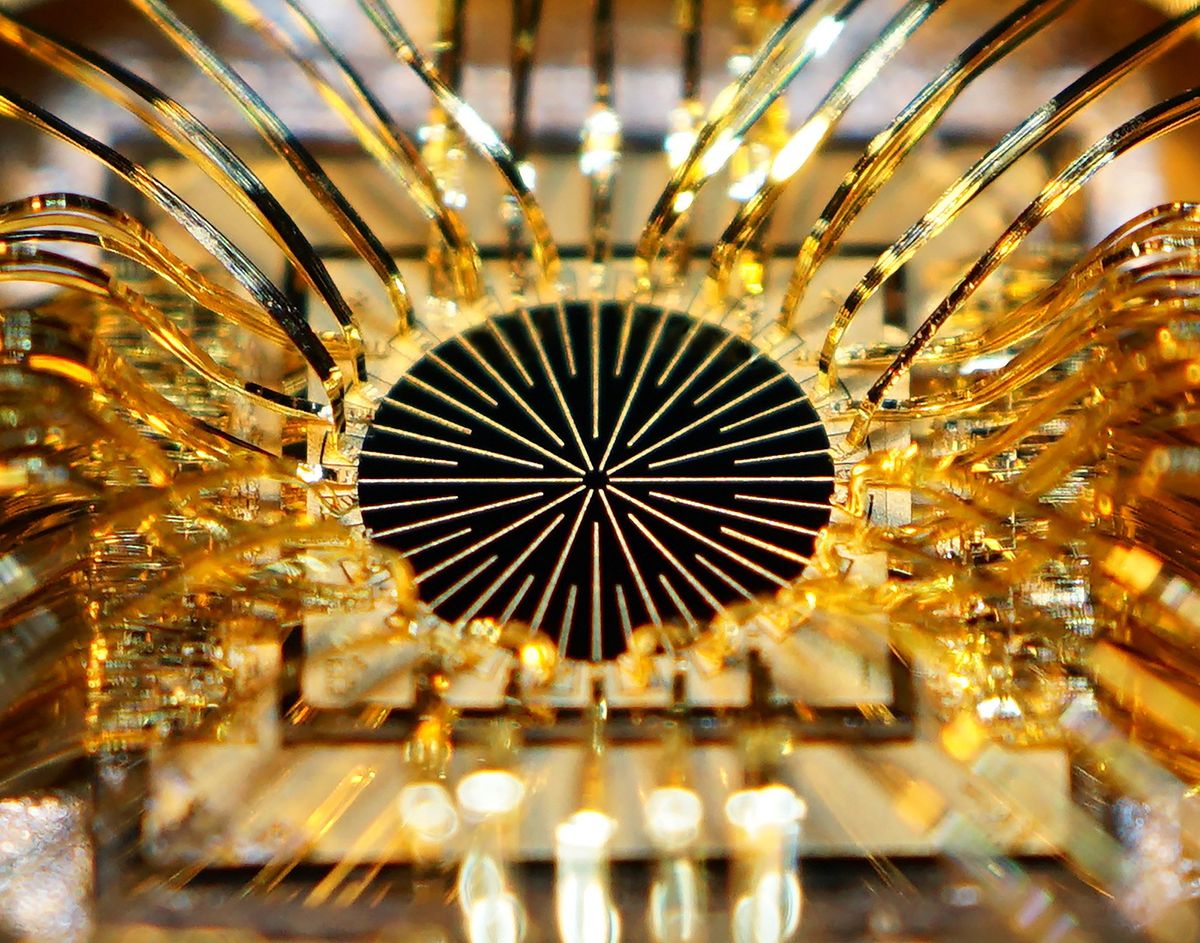
In conventional NMR machines, atoms aligned in a magnetic field are vibrated using a radio-frequency signal in order to measure their oscillation frequency. Those machines require large, powerful magnets.
In T2 Bio’s miniature NMR device, the magnet can be smaller because the sample volume is tiny and because the system measures how quickly the atoms’ vibrations decay instead of their frequency. Specifically, the instrument probes water molecules in a sample. Magnetic nanoparticles coated with antibodies that bind to the target molecule are added to the sample. If the target molecule is present in the sample, the nanoparticles cluster around the target, changing the signal decay rate.
The FDA approved T2 Bio's diagnostic instrument and a test for Candida yeast that runs on the machine. The test can detect five Candida species that cause potentially fatal bloodstream infections. Clinical trials in over 1,500 people showed that the T2 system could detect Candida yeast with 91.1-percent accuracy, a major improvement over blood culture-based tests, which are 60 to 70 percent accurate.
A typical Candida-infected patient stays in the hospital for 40 days at a cost of over $130,000, states the company's website. Doctors usually put patients on antifungal drugs while waiting for blood culture results. Getting a result in a few hours would let doctors quickly deliver the most effective course of treatment. The company mentions a study that shows that providing the right antifungal therapy within 24 hours of symptom onset decreases the length of hospital stay by approximately ten days and decreases the average cost of care by approximately $30,000 per patient.
But the FDA doesn’t recommend replacing blood culture tests yet. Per the agency: “because false positive results are possible with the T2Candida, physicians should perform blood cultures to confirm T2Candida results.”
T2 Bio plans to charge between $150 and $250 for the test, according to this Xconomy article. The challenge the company now faces is to get hospitals to buy their machines and adopt its tests as part of their standard routine.
Prachi Patel is a freelance journalist based in Pittsburgh. She writes about energy, biotechnology, materials science, nanotechnology, and computing.