Researchers have engineered an electronic drug delivery tool that pumps seizure-stopping molecules directly to the source of the problem in the brain. The device, reported yesterday in the journal Science Advances, offers an alternative to conventional, systemic drugs that can cause unwanted side effects throughout the body.
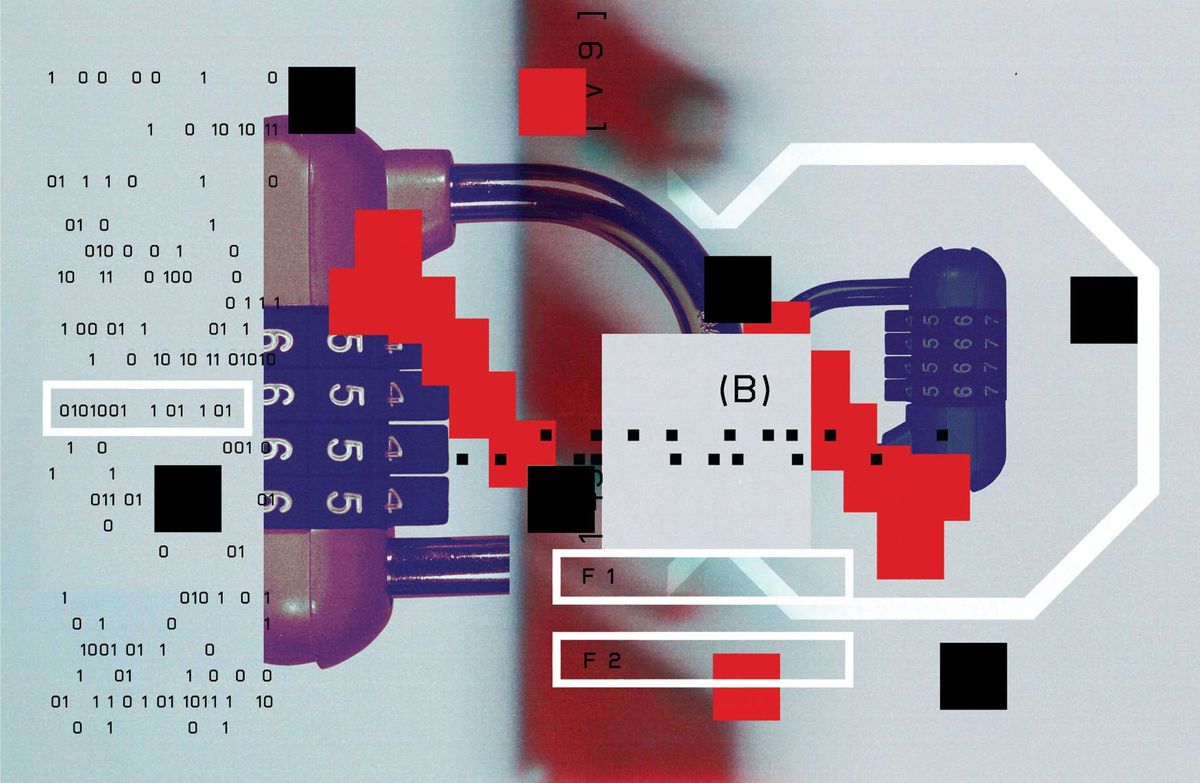
The device, a microfluidic ion pump, uses an electrical potential to move drug molecules from a reservoir on the device across a short channel and out the tip of the device. The pump can be implanted in the brain at the site of a problem, such as a focal point of a seizure, where it will deliver the drug when needed.
The pump technology is based on the concept of electrophoresis: the transport of molecules through a fluid or gel under the influence of an electrical field. When a voltage is applied, electrons withdraw from the source electrode, and positively charged ions—in this case positively charged drug molecules—are driven out of the reservoir, across the ion-conducting membrane, and out of the device for delivery.
The technology builds upon a similar tool developed in recent years called an organic electronic ion pump, which was designed to deliver drugs to the spinal cord and other areas of the body. An improved version of that tool later proved capable of delivering molecules to multiple points in a manner that aims to mimic the speed of neural signaling.
The latest device is smaller and more energy efficient than past designs, making it suitable for use in the brain, says Christopher Proctor, a bioengineer at the University of Cambridge, who helped develop the pump.
“In this research field we’ve been discussing therapeutic applications— particularly in deep brain—for years. This group finally demonstrates that it can really work,” says Daniel Simon, an associate professor at Linköping University in Norrköping, Sweden, who co-developed the earlier organic electronic ion pump technologies, and was not involved with Proctor’s report. The new experiments are a “compelling statement of the utility of electrophoretic drug delivery,” Simon says.
Incorporating microfluidics into the design was key to improving energy efficiency, says Proctor. “That enabled us to significantly decrease the amount of energy needed to drive ions out of the device,” he says. His team’s tool operates on less than one volt, compared to the more than 20 volts often required in previous designs.
Proctor says the new tool is nearly 100 percent efficient, meaning almost all of the ions coming out of the reservoir are drug molecules, instead of a mix of drug molecules and the solvent with which it is mixed.
Electrophoretic drug delivery tools offer a significant advantage over conventional syringe injections, which deliver drugs with considerable force. That puts pressure on delicate brain cells and can cause damage. The technology also offers advantages over systemic drugs delivered orally or intravenously, which disperse throughout the body and can cause side effects.
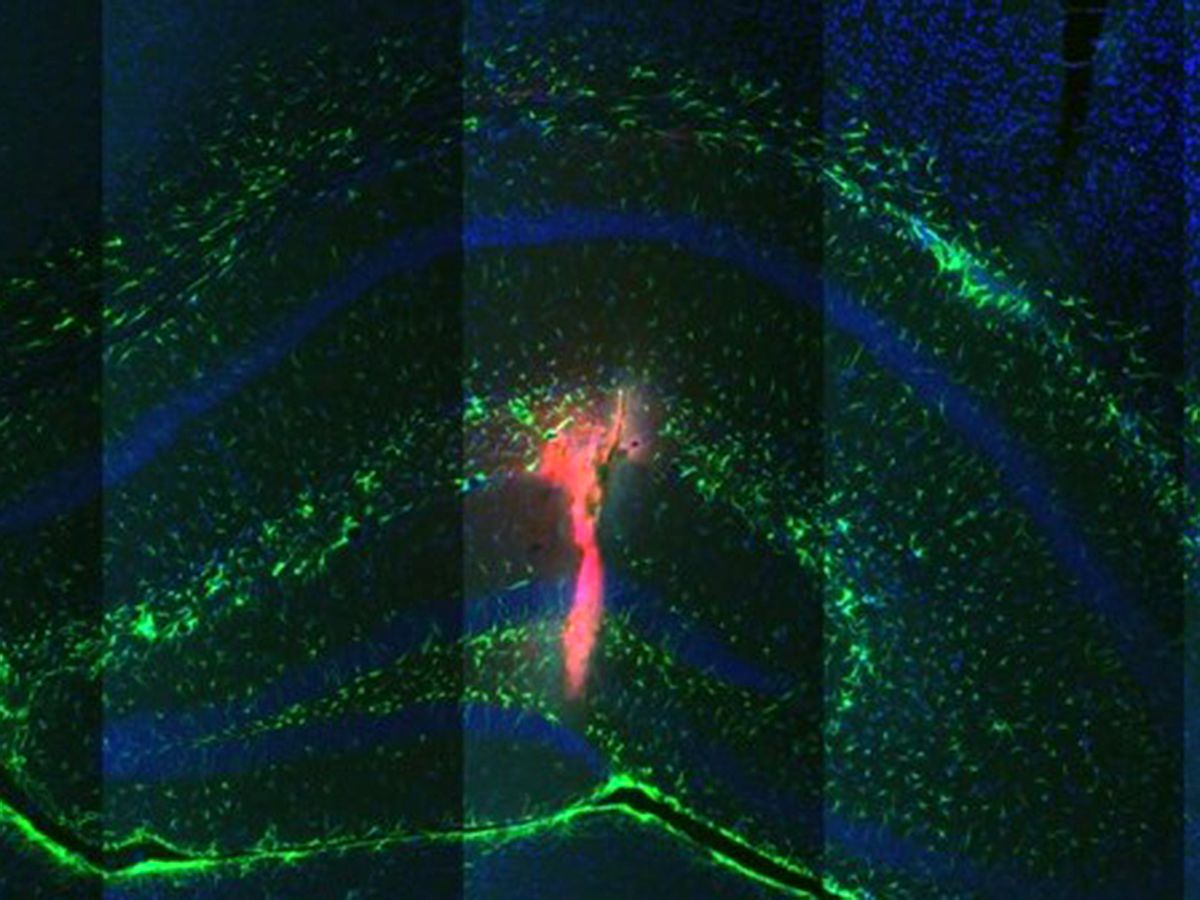
To test the new device, Proctor, and his colleagues at the Institut de Neurosciences des Systémes at Aix Marseille Université, in France, implanted it in the hippocampus of 17 mice. The researchers induced seizures in the anesthetized mice, and then used the microfluidic ion pump to deliver GABA (gamma-aminobuyric acid), an inhibitory neurotransmitter, directly to the focal point of the seizure in the brain.
“We wanted to see if we could stop a seizure that’s already started, and, more interestingly, if we could prevent seizure activity all together,” says Proctor. Based on the results of electrical recordings of the mice’s brain activity, the tool worked for both scenarios. “Shortly after we started delivering GABA, the activity recording would go from intense seizures to normal physiological activity,” he says.
In addition to epilepsy, the device could also be used to deliver drugs for the treatment of other brain disorders such as Parkinsons and brain cancer, Proctor says. Next, the his team plans to further engineer the device so that it can be implanted in freely moving animals. That will involve reducing the footprint of the electrical and fluidic connections, and making the implant more flexible to better match the mechanical properties of the brain.
Updated 31 August 2018
Emily Waltz is a features editor at Spectrum covering power and energy. Prior to joining the staff in January 2024, Emily spent 18 years as a freelance journalist covering biotechnology, primarily for the Nature research journals and Spectrum. Her work has also appeared in Scientific American, Discover, Outside, and the New York Times. Emily has a master's degree from Columbia University Graduate School of Journalism and an undergraduate degree from Vanderbilt University. With every word she writes, Emily strives to say something true and useful. She posts on Twitter/X @EmWaltz and her portfolio can be found on her website.