We know that cells are the building blocks of life, and we know about the parts of a cell that make it work, but what do we know about how all those parts make cells work?
Right now, not much.

In the last two decades, scientists have begun to recognize that mechanical functions within cells play important roles in making cells work, but current methods of observing a cell’s mechanical functions have many limitations that prevent us from truly understanding what those roles are. Right now, the only way to observe a cell and measure its mechanical properties is to freeze, dry, or kill it, or to make contact with the cell. However, these methods disrupt the cell’s functionality and, in some cases, destroy the cell, making it difficult to accurately measure and observe the mechanical functions of cells.
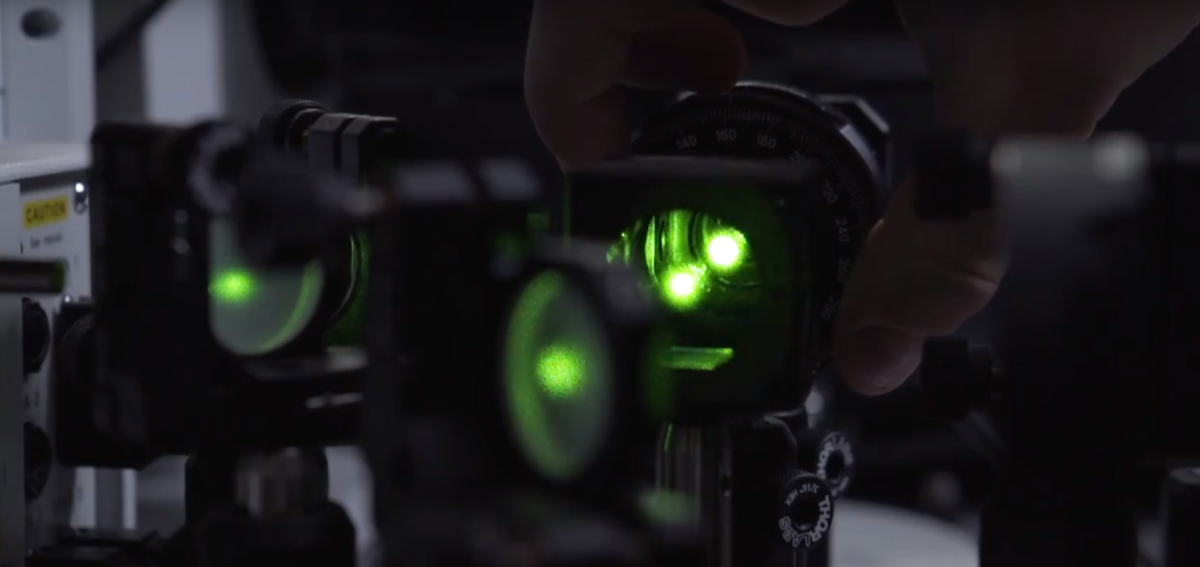
Researchers at the University of Maryland (UMD) are on the case, though, and they have invented a nondestructive and nondisruptive method for observing cells and measuring their mechanical functions using light.
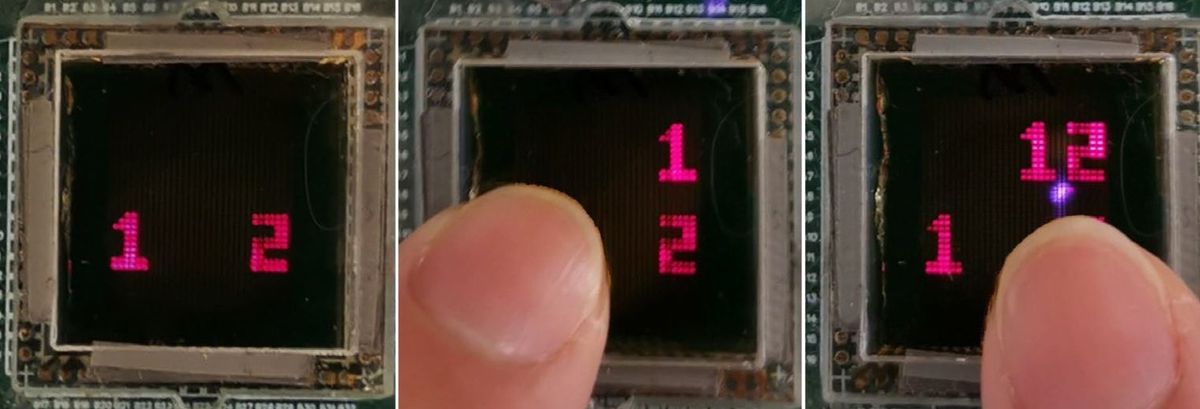
When light hits an object, it changes color, or wavelength, and this change in color can provide information on the mechanical properties of the object the light hits. This process is called Brillouin scattering. The research team has invented a high-resolution module, “Brillouin Scattering Retrofit for Confocal Microscopes,” which can be attached to microscopes and which allows them to quickly measure wavelength changes after light passes through a cell without interfering with the cell’s function.
Understanding how mechanical properties affect a cell’s function is key to understanding many diseases, making the team’s work important to diagnosing and treating disease.
“We are currently blind to the ‘mechano-biology’ universe, with negative consequences to our understanding of many diseases,” says Giuliano Scarcelli, Assistant Professor in the Fischell Department of Bioengineering (BIOE) within the university’s A. James Clark School of Engineering, and one of the inventors of this technology. “By providing a non-perturbative method to characterize cell mechanics, we can begin to fill this important gap.”
The invention team includes Scarcelli; BIOE post-doctoral researcher Jitao Zhang; and Milos Nikolic, Ph.D. student in both BIOE and the university’s Institute for Physical Science and Technology (IPST).
The team is currently working to form a startup company to further develop and manufacture the invention. They plan to design the module to fit existing microscopes so that biomedical researchers can use it with equipment they already have.
“Light-matter interaction is a fascinating topic that we study at a fundamental level,” Scarcelli says. “When applied to biomedicine, it provides new ways to measure important information without labels and without contact — only with light.”
For years, the team – along with other members of Scarcelli’s Optics Biotech Lab – has applied Brillouin spectroscopy to study disease pathogenesis and cancer metastasis. Earlier this year, in fact, Scarcelli was awarded a five-year, $2 million National Institutes of Health (NIH) Research Project Grant (R01) to use Brillouin spectroscopy to improve diagnosis and management of keratoconus, a progressive eye disease that often begins during a person’s teens or early 20s.
More recently, Scarcelli joined forces with researchers from the University of Houston and the Baylor College of Medicine to develop a new approach for investigating a leading cause of birth defects.
In the first few weeks of pregnancy and often before a woman even realizes she’s pregnant, an embryo will have already developed a neural tube, a hollow structure made of cells that will eventually become the brain and spinal cord. Now, with $3.2 million from the National Institutes of Health, Scarcelli is part of an effort to tackle the evolutionary anomaly of why the neural tube closes in most embryos but remains open in others, leading to birth defects such as spina bifida and anencephaly.
Neural tube defects are the second most common structural birth defect in humans, affecting upwards of 500,000 pregnancies worldwide and approximately 2,400 pregnancies each year in the United States.
Embryonic development involves the interplay of driving forces that shape the tissue and the mechanical resistance that the tissue offers in response. However, tissue biomechanics is not well understood because of the lack of techniques that can quantify the stiffness of tissue in high resolution and without manipulating or damaging the tissue.
Led by Professor Kirill Larin of the University of Houston and together with Professor Richard Finnell of the Baylor College of Medicine, the research team including Scarcelli will create new technology combining Brillouin spectroscopy and optical coherence tomography (OCT) to deliver 3D images of the mechanical factors at play when the neural tube closes and—in so many cases—when it does not.
Most commonly used to examine the retina, OCT is an imaging technology that uses light waves to take cross-section pictures. Brillouin spectroscopy is a light scattering technology that will sense tissue mechanical properties, which growing evidence has suggested is critical to the neural tube’s success in closing. Scarcelli has invented and led the development of Brillouin microscopy over the past 10 years.
“Generally, to characterize the stiffness of a material, you need to stretch and pull that material—which usually destroys it. This new Brillouin technology enables us to determine the mechanical properties of embryonic tissue in a noninvasive way and as that tissue grows,” says Scarcelli.
The work fills a significant data gap in understanding neural tube closure biomechanics. The research team says it could have a dramatically positive impact on our understanding of neural tube defects and drive novel treatments for at-risk embryos.
“It’s still one of the great mysteries of life—no one on Earth knows how this happens, and that is really exciting to us,” says Larin, “because we will be the ones to find out.”
Read about related optics research at Maryland.
Receive the latest engineering news from the Clark School in your inbox.