Extending Healthcare's Reach
Telemedicine can help spread medical expertise around the globe
This is part of IEEE Spectrum's special report: Critical Challenges 2002: Technology Takes On
The well-being of tomorrow's patients demands changes in the healthcare structure of today. So says a committee of experts from the U.S. Institute of Medicine (IOM), Washington, D.C., in an analysis of the state of U.S. healthcare in 2001. If even now the system cannot consistently get the right care to the right patients, "we may conclude that it is even less prepared to respond to the extraordinary scientific advances that will surely emerge during the first half of the 21st century," the IOM study warns.
Besides the failure to disseminate medical knowledge fast enough or to use it in a methodical manner, there is another shortfall: medical practitioners with scarce, specialized knowledge cannot bring it to bear beyond their geographical confines.
But technological solutions, telemedicine in particular, are being implemented right now that can spread critical medical expertise across a region and around the globe. For example, a U.S. company believes that the shortage of physicians specializing in intensive care can be mitigated by its telemedicine system. In September 2001 the performance of transatlantic surgery by remote control proved that, with the right equipment, surgeons can perform and teach advanced procedures from thousands of kilometers away. Finally, in the nations and territories of the Pacific Rim, healthcare information networks are granting the region's widely scattered citizens new access to medical expertise.
Air traffic control for intensive care
In the course of over 15 years of practice in intensive care units (ICUs), Drs. Brian Rosenfeld and Michael Breslow slowly realized they didn't have to be there. They were certainly needed--the effectiveness of the ICU specialist, known in the field as an intensivist, is well documented, yet only a third or so of the patients in U.S. ICUs ever get to see one.
As Rosenfeld pointed out, the bulk of the intensivist's job is analyzing physiological data, like electrocardiograms and blood pressure readings, and coordinating care with the surgeons, primary care physicians, respiratory therapists, and others involved in a patient's treatment. That data is available electronically, and the coordination of care can be done remotely with telecommunications.
In a trial at a hospital (one of many) lacking around-the-clock intensivist supervision, the two specialists and their collaborators set out to prove their point. They fed audio, video, and physiological data, as well as treatment records from the hospital's ICU, to a remote site. There, intensivists monitored patients' vital signs and coordinated their care, periodically making virtual rounds by video at any time of the day or night. The hospital's usual ICU staff delivered the hands-on care in the 10-bed facility. Thanks to the round-the-clock expert supervision, the results were dramatic: mortality just about halved, a typical stay in the unit was cut by 28 percent, and the incidence of complications fell by 40 percent. (All the comparisons were adjusted for the severity of the patients' conditions for a proper analysis.) Thanks to the shorter stays and fewer complications, the cost of running the unit fell by one-third. In the four months that the trial ran, "we never set foot in the place," said Rosenfeld.
Armed with these statistics and some venture capital, the two doctors set up Visicu of Baltimore, Md., which proposes to run multiple remote ICUs from a single control center, 24 hours a day, seven days a week. Already it is running an all-electronic ICU (eICU) in Norfolk, Va., a remote site serving units in five hospitals in the region [see figure]. "To a certain extent [this] is air traffic control for patient care," said Rosenfeld. With one physician managing up to 25 patients at one time, the hope is that the company can better distribute the talents of the few intensivists there are. "The reality is that to cover the ICU patients in this country24 hours a day, seven days a week, would take 35 000 intensivists, and we only have about 5500 in active practice now," said Rosenfeld. "And that 35 000 is assuming you could get that many to work nights and weekends."
Although it is only one of several solutions to the shortage, such telemedicine has merit, according to Dr. Ann E. Thompson, president of the Society of Critical Care Medicine, Des Plaines, Ill. "It has a long way to go to demonstrate exactly what its potential is, but it may be a way of spreading a thin resource over a much larger population," she said.
The technique also has some limits. "We don't know yet how widely applicable the approach can be, nor do we know how many centers or patients an intensivist can observe at one time using telemedicine," she noted. "Another limit is that you must have people present in the ICU who have the technical capabilities to effect the specialist's recommendations. Interestingly, it is easier to find someone technically competent than someone who can recognize that the patient is developing a difficulty and who knows the right moment to intervene. But you need both."
Professional guardrails
Visicu has built two software systems to utilize all the data streaming from the ICU, both of them based on access to electronic patient records. The first system will trigger alarms to alert the intensivist to impending trouble with a patient. It consists of algorithms that track each patient's physiological data and laboratory results, all of which are stored in an electronic patient record at the eICU. Should the data values pass patient-specific thresholds that might point to a turn for the worse, the staff there will be alerted by the software well in advance of the need for intervention.
The second is a decision support system, an interactive set of protocols that help the caregiver decide on a treatment on the basis of the best practices for particular conditions. Use of such clinical decision support tools is on the rise, particularly as hospitals abandon paper records and handwritten prescriptions in favor of electronic medical records and physician order entry systems. By reminding physicians of the established procedure for a given situation, these tools act as what Dr. Daniel R. Masys, director of biomedical informatics at the University of California at San Diego, calls "professional guardrails."
Such guardrails work even when they are not electronic. Dr. Brent James, executive director of the Institute for Health Care Delivery Research in Salt Lake City, Utah, demonstrated this with a heart medicine. Doctors' proper use of the therapy jumped from 48.8 percent to 95 percent at his hospital when a checklist spelling out the best practice protocols for the drug's use was added to the patient's discharge summary. Integration into an electronic patient record makes a difference in two ways, according to James. First, many more protocols can be put in place in an electronic clinical information system than on paper. "The maximum number of paper protocols we were able to introduce is four," he said. "The paper overwhelms." Second, an automated system with electronic patient records allows physicians to more easily refine the protocols and develop new ones.
ICU engineering
The eICU is typical of many information technology projects in medicine. Components need to be robust and of high quality, while security of data and quality of service are also high priorities. A videocamera in every patient's room has to have sufficient resolution and pan, tilt, and zoom features for the remote physician to be able to examine, for example, the pupil of a patient's eye. Patient information has to be well guarded; data inside the hospital runs over a dedicated virtual local-area network within the hospital's own network, and then it is encrypted as it leaves the hospital through a T1 line. Data is decrypted at the remote unit and runs through a virtual network there, too. Should access to the T1 be interrupted, the system automatically switches over to a backup integrated-services digital network (ISDN) line.
All of the technology needed to build the eICU was readily available. The hard part was integration, according to Bill Super, vice president and chief technology officer at Visicu. Between the hospitals and the eICU, 260 separate hardware and software components must be glued up into a system that allows the remote physician to see and hear everything in each patient's room, observe all the medical records and physiological data, and communicate with hospital staff.
As far as technology is concerned, there is little reason an ICU specialist ever needs to be in the eICU itself, accordingto Super. With the proper networking, experts at their homes in Virginia could observe patients in Moscow. "There are actually greater issues in credentialing and licensing physicians than in the technology itself," said Super.
Surgical globe-trotter
Those licensing issues will have to be worked out soon if Dr. Jacques Marescaux, head of the European Institute for Telesurgery in Strasbourg, France, is to have his way. While economists envision the globalization of trade, he envisions the globalization of surgery. Last September, while Marescaux was in New York City, he removed a woman's gallbladder at a hospital in Strasbourg.
In a sense, performing surgery remotely is the extreme of telemedicine technology, demanding the keenest vision and finest touch of any medical procedure. At present, precise and easy-to-use surgical robots and low-latency, long-distance data connections--the technologies to make it work over appreciable distances--are available, although certainly not universally. As telesurgery catches on, Marescaux and others think expertise that once was transmitted in person will spread rapidly, with tangible effects on surgical error rates.
"When a surgeon begins a new operation alone, the first 10-20 operations are on a learning curve, and the complication rate is higher," Marescaux explained. "In the future, if we can suppress that with technology, no one will accept such high rates."
Giving experts the ability to supervise novice surgeons as if they were in the room with them will undoubtedly help, and so-called telementoring networks for endoscopic and laparoscopic surgery already exist. Surgeons at one medical center can watch the video feed from a camera attached to an endoscope or laparoscope at another center and communicate with the surgeon there. A network based at Japan's Osaka University has been in operation since 1997, and others are in development, the intention being to link all Japan in a sort of endoscopic Internet service. But Marescaux hopes that the kind of remote surgery he performed will make a bigger difference, in that an instructing surgeon can actually take control at crucial points.
For the transatlantic procedure, Marescaux used a Zeus robotic surgical system, developed by Computer Motion Inc., Goleta, Calif. In point of fact, Zeus's two major components, a control console and a three-armed robot, were designed to be located together in an operating room. The surgeon moves controls on the end of two arms at a console; these movements are translated to the two robot arms manipulating surgical instruments within thin tubes. The tubes enter the patient's body through pencil-width incisions [see photo]. The third arm maneuvers a videocamera in a separate tube, so that the surgeon may see the other two instruments within the abdomen. The camera operates by voice command. Medical personnel at the patient's side prepare the patient for surgery, make the initial incision, and place the robot arms at the points where they enter the body.
Round-trip race
In many applications of telemedicine, as elsewhere, bandwidth is the limiting factor. That was not the case in the New York-to-Strasbourg surgery. Each of the robot's three arms transmits redundant position signals. Both voice-over Internet protocol (VoIP), for Marescaux to communicate with the personnel at the patient's side, and high-quality video were transmitted, 10 Mb/s of data in all. But that was easily handled by the network supplied for the surgery by France Telecom, Paris. Instead, the time it took a signal to travel from the console in New York City to the robot in Strasbourg and back--the latency--proved the most critical aspect of the network technology.
Indeed, until the September surgery, latency was expected to put what the surgeon sees at the controls too far out of synch with events on the operating table for the technique to be used beyond a distance of about 300 km. Experiments by Marescaux's group found that any latency greater than 250 ms was dangerous, but engineers at Computer Motions and France Telecom compressed it to just 155 ms, "below human brain perception, that was our target," said Christophe Rabadan, team manager at France Telecom R&D. France Telecom supplied the asynchronous transfer mode (ATM) network and optical-fiber channels over which the surgery was performed. ATM was used because it allows control over the quality of service and a constant bit-rate.
A full 70 ms of the latency was taken up by the video coding and decoding from the endoscopic camera. According to Rabadan, use of an advanced coding and decoding system for the video was a big timesaver.
Moji Ghodoussi, who managed the project for Computer Motions, said that the basic hardware and software for the Zeus robot was not changed for the telesurgery, but several components were added to handle the networking and communications between the two sites. Those essentially tricked the controller and the robot into thinking they were in the same room rather than separated by a network and over 7000 km of optical fiber.
"Safety is a big concern," said Ghodoussi. "So there are a lot of checks and balances." Even under the best conditions, data packets can be dropped and errors can occur, but those cannot be allowed to endanger the patient. "If the link breaks, we maintain the last good data," he said. "If a packet arrives out of order, [the robot] just discards it. If the discards are not too many," the system seems to the surgeon to perform seamlessly.
One highly engineered demonstration does not a healthcare revolution make. That will take the proliferation of both surgical robots and reliable, low-latency communications. The first is beginning to happen. Computer Motions has about 50 Zeus systems installed around the world, and its competitor in surgical robotics, Intuitive Surgical Inc., Mountain View, Calif., has over 70. By filtering out tremors in the surgeon's hands, the robots perform laparoscopic surgeries with greater accuracy than is humanly possible.
Telecommunications infrastructure is constantly improving, but its reach outside of the developed world is minimal. To get into developing countries, "we need to have a connection through satellite," said Marescaux. "That's the limit of the technology today." The latency using ATM and a satellite in geosynchronous orbit would be at least 600 ms, three times too long. Whether it will ever make economic sense for a poor nation to invest in a surgical robot is an open question.
The Pacific theater's teleplay
What can you do with an out-of-service weather satellite in a decaying orbit? Provide medical education and consulting services throughout the whole Pacific Ocean.
Headquartered at the University of Hawaii in Honolulu, the Peacesat program uses the GOES-7 satellite and communications assets on the ground to make up for the lack of access to medical expertise and educational resources on islands in the Pacific. Meanwhile, high on a hill across town, the U.S. Department of Veterans Affairs (VA) and the Department of Defense have joined forces to improve access to care for their many beneficiaries in Hawaii and on other Pacific islands. Linked together through the State of Hawaii Telehealth Access Network (STAN), the three are conquering the disparities in healthcare in the Pacific.
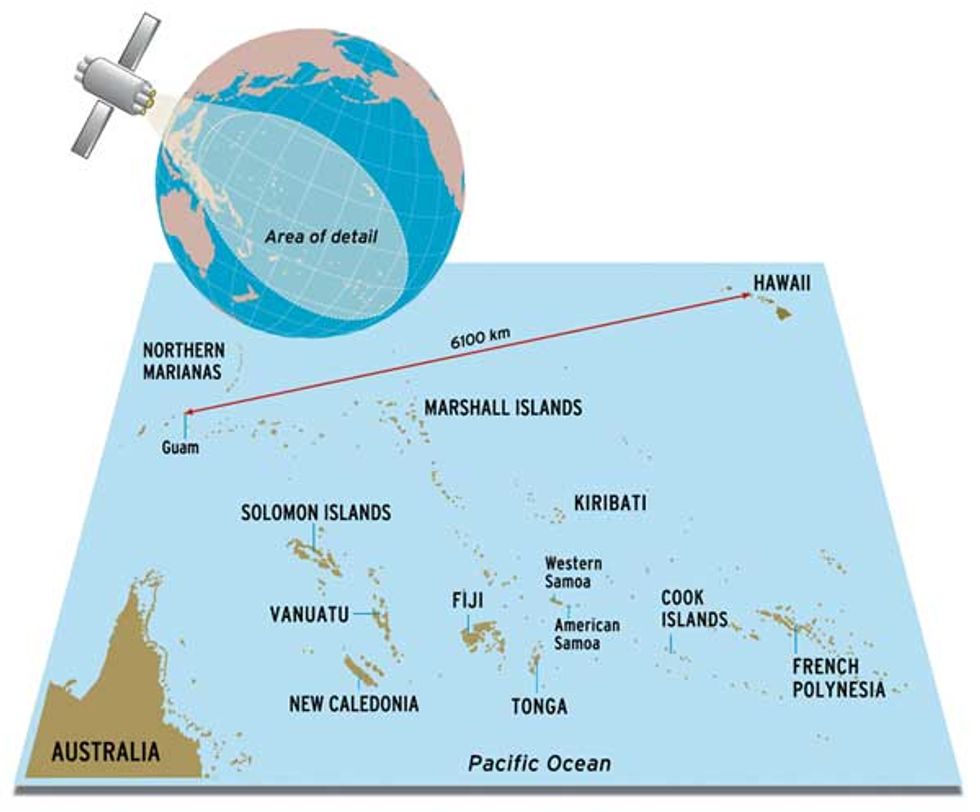
It is a challenging goal. "Everyone is trying to beat space and time," said Major John R. Ewing, director of Defense Department operations for the Pacific Telehealth and Technology Hui (Hawaiian for "group"), which is based at Tripler Army Medical Center, in Honolulu. The Pacific takes up a lot of space and hence has many differences in local time [see illustration, top]. The islands there span more than five time zones. One of the farthest linked to the Hawaiian centers, the U.S. territory of Guam, is 6100 km from Hawaii and shares no working hours with the continental United States. Telecommunications facilities in the region are sparse and enormously expensive, and the South Pacific islands are hardly well off economically.
Begun in 1971, Peacesat is now operating its fifth weather-cum-communications satellite, the 14-year-old GOES-7. Provided by the U.S. National Oceanic and Atmospheric Administration, Washington, D.C., the satellite has outlived its usefulness to that organization. Instruments on board have been superseded by better sensing technology and the fuel to maintain a perfect orbit is lacking. GOES-7 is already orbiting at a five-degree inclination to the equator, tracing a figure eight in the sky. In another 10 years it will be incapable of holding a useful position and will have to be brought down by ground controllers. Since it was not designed as a communications satellite, GOES-7's bandwidth is less than ideal, but it is enough to provide 128 kb/s for videoconferencing and 64 kb/s for Internet connectivity, plus nine simplex audio channels. Today, 52 transceivers in 22 Pacific island nations and territories spanning an area equal to one-third the earth's surface use GOES-7 as a conduit to Hawaiian and U.S. mainland medicine as well as educational and government services.
Points to Ponder
ORIGINS Telemedicine began in earnest in the 1960s to meet NASA's need to monitor orbiting astronauts' vital signs.
INSTALLED BASE According to a United Nations study, 1600 medical robots were in use in 2000 and an estimated 4800 more will be installed by 2004.
The satellite, in turn, is linked to a variety of other networks through the government network, STAN. "We run every kind of protocol and every kind of link--ATM, frame relay, ISDN--and we support all video [protocols]," said Norman H. Okamura, who manages the program. "In every location, what is most cost effective is going to vary from site to site." Some islands, such as American Samoa, have separate datalinks to Peacesat, such as T1 lines, but others, like the Federated States of Micronesia, rely entirely on the GOES-7 satellite.
Ray Tulafono videoconferenced with IEEE Spectrum over the network from the Lyndon Baines Johnson (LBJ) Tropical Medical Center on American Samoa. He said that doctors there used Peacesat for continuing education, consultations with experts at Shriners Hospital in Honolulu, patient follow-ups, and more. Shriners has treated over 2000 Pacific island children in Honolulu with valuable aid from the telemedicine project, according to Jana Chang, who runs the program at Shriners. Without Peacesat, children and their guardians would have to be flown to Honolulu and given a place to stay in order to do follow-up procedures.
Military medicine
Across town from Peacesat, at the Pacific Telehealth and Technology Hui, the VA is also in the thick of telemedicine projects. These involve videoconferencing for evaluating post-.traumatic stress disorder, digital imaging to do dermatology consultations, and the installation of network-connected monitors for vital signs in the homes of veterans in rural areas.
According to Dr. Stanley M. Saiki Jr., the Hui's director, electronic patient records are "the backbone" in much of telemedicine. They give a consultant a view of the entire patient history. "The consultant theoretically has a greater breadth of experience and may see things that aren't obvious to you," he observed. The VA is currently migrating its own, well-respected, electronic medical record system to the Lyndon Baines Johnson Tropical Medical Center on American Samoa to care for veterans on that island.
The Defense Department's telemedicine work is oriented more toward experiment and prototyping than is the VA's, and its telemedicine projects have not always been successful. Such was the case with the Theater Telemedicine Prototype Project (T2P2), designed to allow a medical technician to receive expert consultations from physicians thousands of kilometers away.
Technologically, it was a success, but it only proved useful if there were barriers to care, as when a soldier must receive care in the field, said Major Ewing. But, since in peacetime medics can consult physicians in person, they were not using the system. And, under the military's train-as-you-would-fight philosophy, "if you're going to use teleconsultation in a war environment, you should use the same system in your day-to-day environment," he said. However, building on the experience and technology of T2P2, the Hui is developing an electronic consultation mechanism that should be useful for both the VA and Defense Department clinics in the Pacific.
To Probe Further
For a broad view of how to improve healthcare systems, see the Institute of Medicine's "Crossing the Quality Chasm: A New Health System for the 21st Century," available from the National Academy Press, Washington, D.C., or free on-line at https://www.nap.edu.
The Telemedicine Information Exchange offers a clearinghouse of articles and developments in telemedicine. See details on the Exchange's Web site at https://tie.telemed.org
More information on remote and robotic surgery, including the New York-to-Strasbourg surgery mentioned in the article, is available at https://www.websurg.com.