GlaxoSmithKline is the world’s sixth largest pharmaceutical company, and last year it racked up sales of $33 billion for its pills, powders, vaccines, and consumer products. Yet in a one-on-one conversation with IEEE Spectrum, GSK executive Moncef Slaoui dismissed all these profit centers as the old way of medicine.
Slaoui has led GSK’s major research effort in “electroceuticals,” in which devices treat diseases by sending electric pulses through the body’s nerves. As nerve cells communicate naturally via electric pulses, this technique tries to speak the native language of the nervous system. In an interview with Spectrum before his talk at SXSW Interactive on Friday, Slaoui said he’s convinced that doctors will soon be prescribing such treatments: “The only question is, how many different disease will be treated with bioelectric medicine?”
Since 2013, GSK has funded research at 50 labs and startups, Slaoui said, and it’s now planning clinical trials for implanted devices that will provide bioelectric treatments for three chronic diseases. He wouldn’t disclose specifics, saying only that the three conditions include one autoimmune disorder and one metabolic disease. He would say that the company expects to start trials in 2017 and have results within three years.
Currently, GSK is focused on devices that will be implanted on peripheral nerves in the body; controling signals in the brain is “orders of magnitude” harder, Slaoui said. But working with peripheral nerves that lead to major organs provides plenty of opportunities to treat chronic diseases. Slaoui rattled off a list of ailments that included obesity, hypertension, type 2 diabetes, asthma, and arthritis.
So what do electroceuticals offer that pharmaceuticals don’t? More precisely targeted treatments, Slaoui said. When you take a chemical medicine, you’re taking in a 3-D molecule that’s designed to only fit with one particular receptor in your body, and therefore only affect that one body part. “Then you drown the body in that molecule, and you hope that it only fits that [receptor],” said Slaoui. If it impacts other parts of the body, you get side effects.
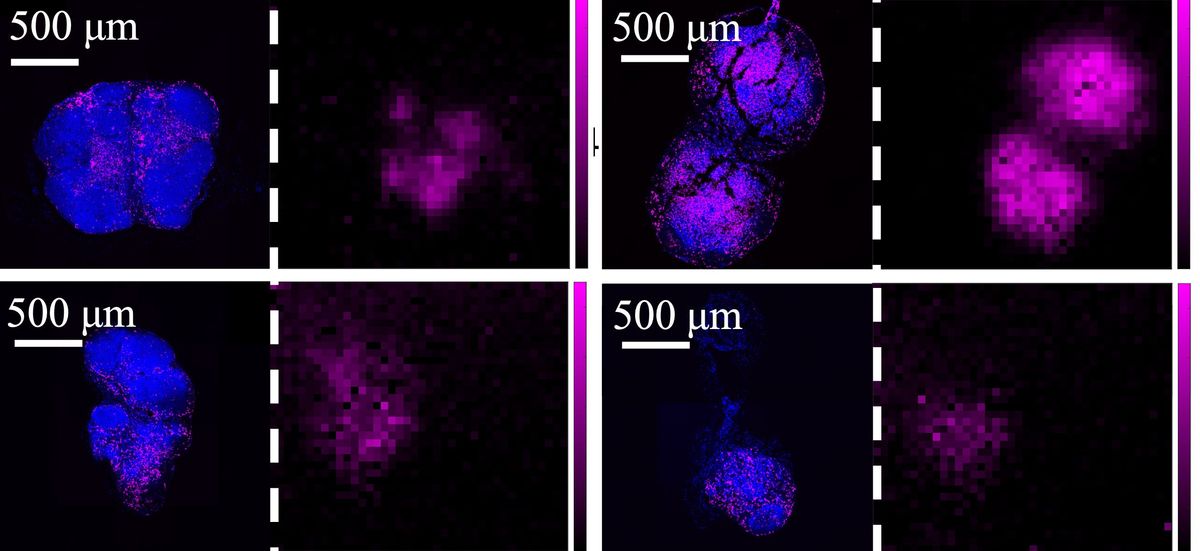
In GSK’s vision of bioelectronic medicine, the effects are inherently localized: Doctors would implant a tiny electrical device on a nerve leading only to the organ they want to impact, such as the kidneys or the spleen. The device could also provide more precisely timed treatments: It could record signals from the nervous system and send its pulses down the nerve only when needed, whether that’s many times a day or once every few weeks.
GSK is hardly alone in researching bioelectric medicine. Spectrum has covered many companies that are building electronic devices to stimulate the vagus nerve, a major nerve that winds through the body and sends signals to organs such as the heart, lung, stomach, and intestines. (This interactive graphic shows how vagus nerve stimulation works.) Traditional medical device companies like Medtronic already sell electronic implantables that work with the nervous system, including the neurons in the brain.
GSK is trying to catch up by partnering with academics and startups. Many of these partnerships have come about thanks to the Big Pharma company’s Bioelectronics Innovation Challenge, which will award $1 million to a team that produces a miniaturized, fully implantable device that can attach to a nerve and send an electrical signal to a single organ. Slaoui says three finalist teams are now vying for the prize (though he wouldn’t say who they are), and he hopes to declare a winner within the next 12 months. But it’s worth noting that the prize was announced in 2013, and in 2014 GSK decided to go ahead and give money to teams working on the problem. Clearly, it’s not an easy assignment.
The challenges of creating such a device are many: It must have a miniaturized chip and tiny electrodes that can interface with a single nerve; its materials must be compatible with a human’s soft and squishy insides; and it must have a wireless way to receive power—traditional batteries are out, Slaoui says, because they generate too much damaging heat.
Let’s assume that a team does create such a device. What, then, will determine whether they become part of mainstream medicine? One open question is how these devices will be implanted. “We want to make bioelectric medicine something that happens in the doctor’s office rather than the hospital,” Slaoui says. He envisions tiny surgical robotic tools that can be inserted laproscopically to place the devices inside patients. “You punch a little hole, and [the robotic tool] uses a “smart” head with a camera to find its way to the viscera, then a tool grafts the electrode to the nerve,” he says. In GSK’s vision, biolectronic medince thus becomes no big deal. “You can walk out 10 minutes later,” Slaoui says.
Eliza Strickland is a senior editor at IEEE Spectrum, where she covers AI, biomedical engineering, and other topics. She holds a master’s degree in journalism from Columbia University.