Herek Clack gets an email notification each time someone calls his office phone at the University of Michigan. He says that while working from home during the pandemic, his office phone has been ringing “continuously.” Meanwhile, online, one of his studies is trending as the most-read paper in Journal of Physics D: Applied Physics, despite being published more than a year ago.
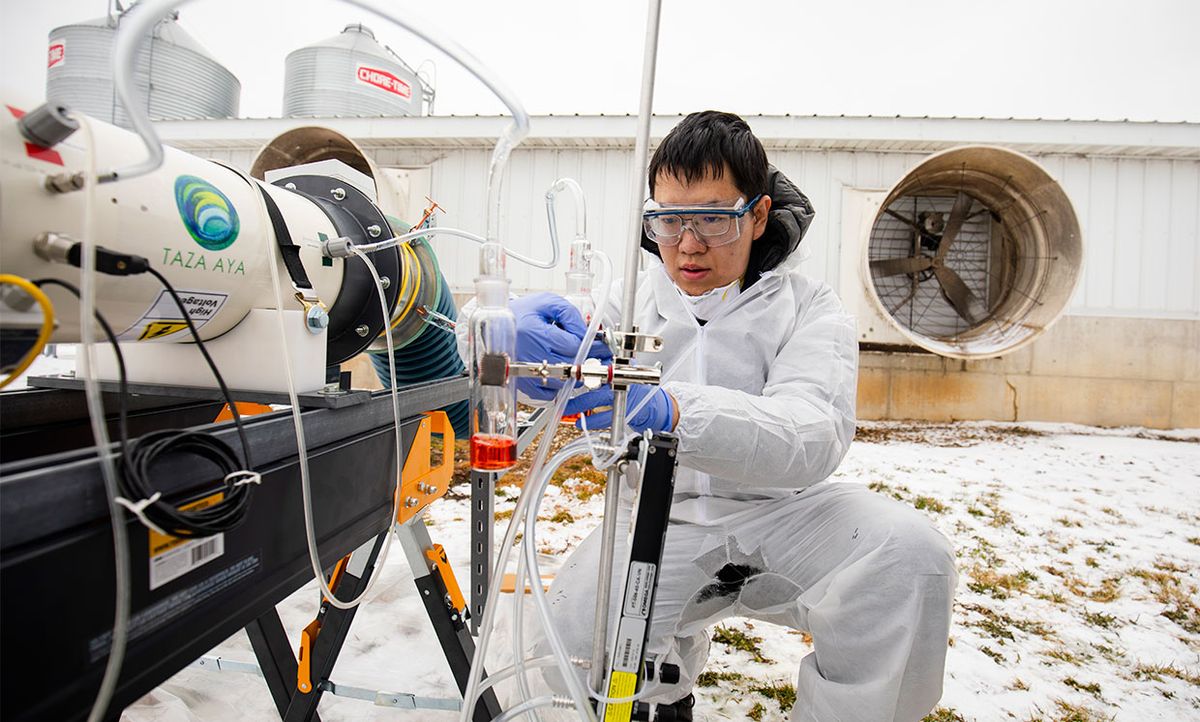
Part of Clack’s research is focused on using nonthermal plasma as a means to inactivate airborne viruses. His team demonstrated this technique against MS2, a virus that infects bacteria and is known to be particularly difficult to inactivate. In a second study, Clack proved that nonthermal plasma could also inactivate the porcine reproductive and respiratory syndrome virus (PRRSv), which affects pigs. Now, many curious people are reaching out to Clack with the same question in mind: Could nonthermal plasma inactivate the novel coronavirus, SARS-COV-2?
Plasma is a state of matter in which high enough energy levels cause electrons to be knocked out of their orbits and enter a free state. Unsurprisingly, these radical electrons can be damaging to DNA and RNA. The ability for nonthermal plasma to disrupt the infectiousness of a virus was first demonstrated by a group of Chinese researchers in 2015, and Clack’s team has since been exploring its potential use to deactivate viruses in the agricultural setting. Their idea is to incorporate nonthermal plasma devices into the ventilation systems of pig farms, to limit the spread of infectious diseases like PRRSv.

Clack says the exact mechanism by which the plasma deactivates these viruses is still being explored. “But the thinking is that it interrupts the ability for the virus to dock with its host cell,” he says. “Our studies show that the number of infectious virus dropped more than two log, so more than 99 percent if you compare before-and-after plasma treatment.”
While the ability of both MS2 and PRRSv to infect cells was substantially reduced in Clack’s studies, the overall amount of viral genetic material was hardly affected. This suggests that nonthermal plasma, at just the right intensity, may be altering the proteins on the surface of the viruses, which they use to enter their host cells. Without intact proteins, the virus can no longer infect its host cell.
As it became increasingly clear that the novel coronavirus is airborne, and was detected in the air vents of hospitals, more people have reached out to inquire about the applicability of Clack’s research to SARS-COV-2. Could nonthermal plasma devices inside air ventilation systems—for example, in hospitals—help reduce the spread of the virus? Exploring this possibility is intriguing but would be riddled with many hurdles.
“COVID-19 is…highly contagious, with no innate population immunity, potentially deadly health outcomes, and no vaccine in sight—so gaining approval to work with it is not a mundane undertaking,” Clack emphasizes. It would require a carefully regulated study in a Level 3 biosafety lab, which he notes is expensive and difficult to gain clearance for.
Nevertheless, the possibility of pursuing such a study has crossed his mind.
The major question, Clack notes, is where in the queue of many scientists, with many COVID-19-related research questions, does this potential study fall? Research to find a vaccine is clearly a priority but may also take some time to develop and implement. In the meantime, Clack points out, our only protection against the virus is social distancing, face covering, and self quarantine. “And so that’s where our technology really could have the most impact—by providing protection where the vaccines aren’t yet ready,” he says.
Despite the need for more ways to combat SARS-COV-2, the challenges of using nonthermal plasma in the context of the current pandemic may prove too cumbersome. The high queue of COVID-19 research proposals, the need for FDA approval of nonthermal plasma devices in human settings, and limited ways to produce such devices for air ventilation systems remain major short-term barriers.
Michelle Hampson is a freelance writer based in Halifax. She frequently contributes to Spectrum's Journal Watch coverage, which highlights newsworthy studies published in IEEE journals.