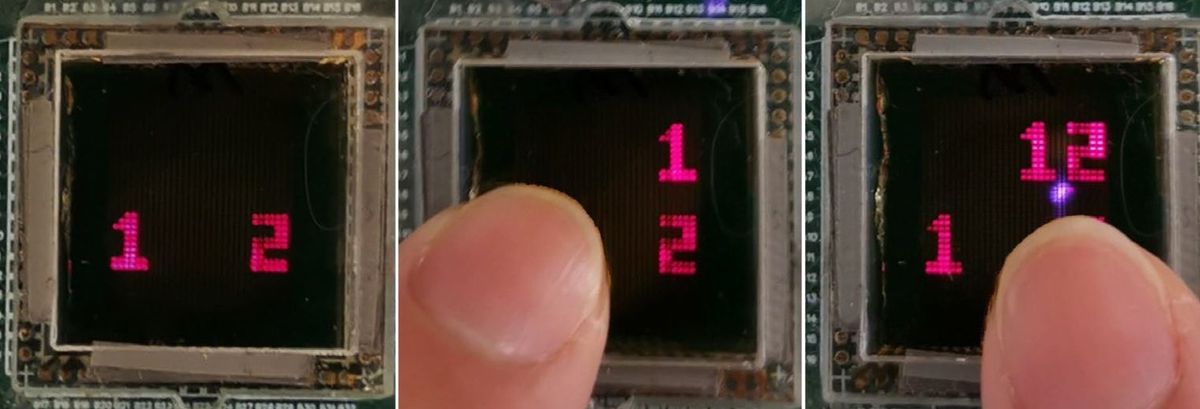
The device pictured above, the Chattanooga Intelect TranSport, was used in experiments to determine whether ultrasound would be an effective contraceptive technique for monkeys.
Researchers have long sought new methods for male contraception beyond the condom and the vasectomy—in other words, the male equivalent of the birth control pill. Now separate research teams at the University of North Carolina (UNC), the University of California, Davis, and the University of Bari in Italy have shown that irradiation with ultrasound of the type that sports medicine specialists use to bring relief to aching joints can painlessly shut down sperm production.
(What can’t ultrasound do? IEEE Spectrumhas reported on breakthroughs using ultrasound for mind reading, controlling Parkinson’s and other neurological ailments, and curing migraines and depression)
According to Dr. James Tsuruta, who headed the UNC team, finding the right combination of ultrasound power, frequency, and duration to shut down sperm production in rats required a lot of experimentation. Eventually, Tsuruta’s team hit upon a setting for the device and a methodology that resulted in sterilization. They showed that two 15-minute sessions spaced two days apart were enough to cause almost complete eradication of sperm at various stages of development. Instead of placing the ultrasound transducer in direct contact with the testes as is done with, say, a knee or shoulder, the scrotum was placed in a cup of hot salt water that allowed the energy emitted by the wand to be conducted to the skin. Tsuruta and his colleagues, who applied heat to separate groups of mice—some with and some without ultrasound—found that “There is something special about heating with ultrasound; it caused 10-times lower sperm counts than just applying heat,” says Tsuruta.
Asked what accounts for this difference, Elaine Lissner, director of the Male Contraception Information Project and founder of the Parsemus Foundation, which funded the UNC study, said, “This is one of the mysteries that has yet to be solved.” The best guess, says Lissner, is the one ventured by the late Dr. Mostafa Fahim, who, back in the 1970s, was the first researcher to try therapeutic ultrasound for male contraception. Fahim thought that ion transfer involving the salt in the conducting saline had an effect.
(Fahim and colleagues at the University of Missouri in Columbia published journal articles and book chapters and were awarded patents related to their sperm-killing technique. But a more renowned researcher set ultrasound contraception on the backburner for more than two decades when he couldn’t reproduce Fahim’s results.)
The UC-Davis team wanted to see how effective ultrasound would be on larger animals such as primates, so they started right off experimenting with monkeys. And just like the UNC team, zeroing in on the right settings took time and persistence. (They irradiated the testes using a commercially available device called the Chattanooga Intelect TranSport. The UNC rat and the Bari dog studies used different devices that anyone can purchase online.)
"We were pretty discouraged at first," says Dr. Catherine VandeVoort, the UC-Davis team’s lead researcher. "The monkeys didn't seem to mind the treatment a bit, but we were having a rough time of it. Thirty minutes of treatment three times a week is a lot of monkey testicular massage.”
They eventually found that three 30-minute sessions, each spaced two days apart, was enough to temporarily depress sperm production. But sperm counts would return to normal after about six weeks, giving the UC-Davis researchers the idea that they had hit upon a reversible, noninvasive male contraceptive. The main problem with that, say observers, is that a man would find it difficult to be certain exactly when his temporary sterility has worn off.
The two U.S. teams were aware of each other’s work. But they had no idea that Raffaella Leoci, a veterinary researcher, had come up with the same killer app for ultrasound at the behest of a German company. Having stumbled upon Fahim’s papers, Leoci reasoned that “We have a big problem with stray dogs here; if it really worked, that might be a more humane and affordable way to sterilize them than surgery.” Leoci’s experiments proved that three 5-minute treatments, each spaced two days apart, were enough to permanently sterilize a dog.
“The UNC team's rat study has the numbers, and they have beautiful histology data showing what's going on inside the testes,” says Ted Tollner, a member of the UC-Davis team. “The Italian team was first to publish and showed ultrasound could be very effective in a large animal, not just rats. Together with our results showing the possibility of reversibility, along with effectiveness in the closest animal to humans, it makes a pretty compelling package.”
Willie Jones is an associate editor at IEEE Spectrum. In addition to editing and planning daily coverage, he manages several of Spectrum's newsletters and contributes regularly to the monthly Big Picture section that appears in the print edition.