I’ve got you under my skin.
I’ve got you deep in the heart of me,
So deep in my heart, you’re nearly a part of me.
Clinical laboratory tests are like snapshot photos: you draw some blood, send it to the lab, and (eventually) get an impression of body’s metabolic condition at the moment the needle pierced the skin. How much cooler it would be if there were something like cell-phone video—a continuous succession of data on the fluctuations of key biological parameters, covering not just a moment or an hour, but weeks and even months. Such a device could transform both medical research and the clinical monitoring of chronic conditions like diabetes.
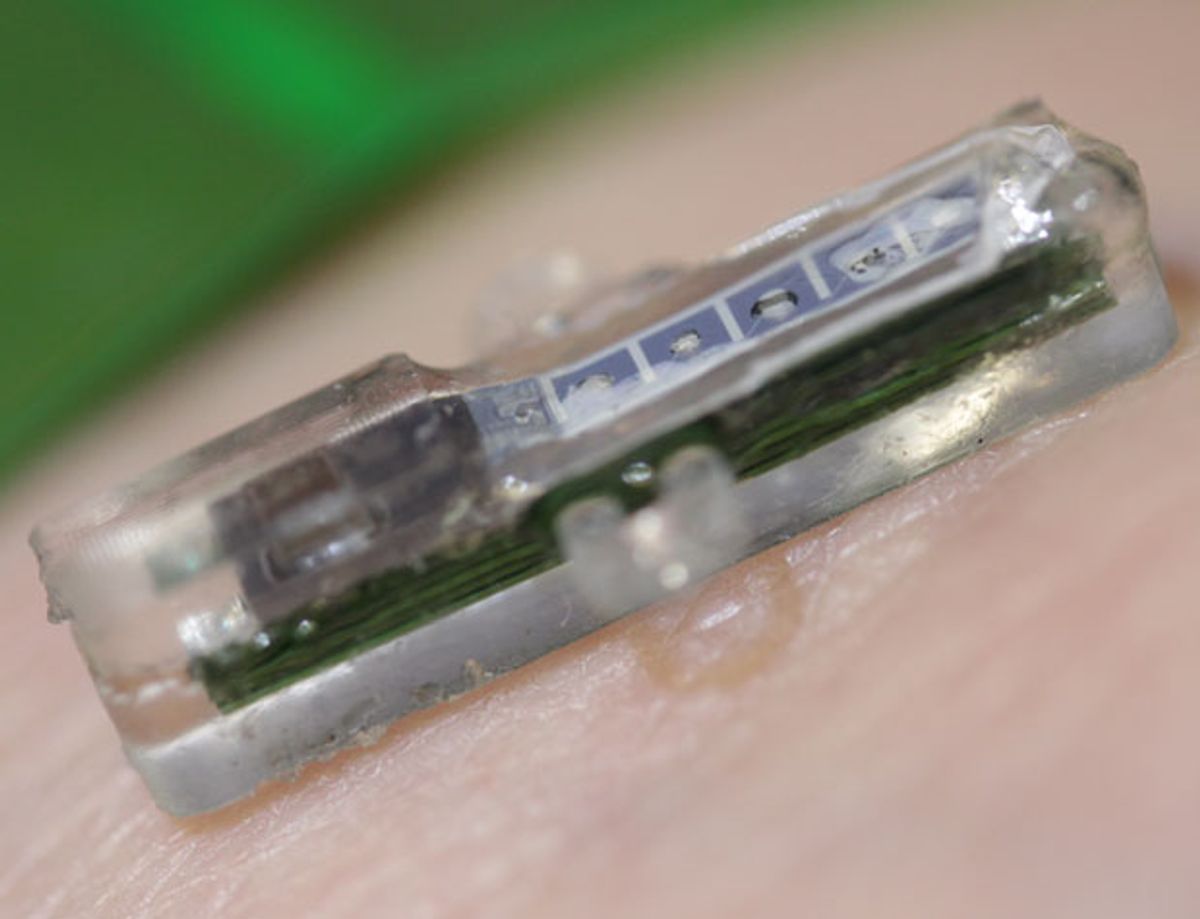
An interdisciplinary team at the Ecole Polytechnique Federale de Lausanne (EPFL) is one of the groups pursuing implantable wireless biosensors. At the Design, Automation and Test in Europe (DATE) conference in Grenoble, France, researchers Giovanni De Micheli, Sandro Carrara, and co-workers reported progress on their i-IronIC biosensor system. The device consists of an implanted miniature laboratory built into a tiny box just 2.2 by 2.2 by 15 millimeters and a skin patch that provides power, controls, and data relays between the patch and a Bluetooth-enabled cell phone.
Into the 0.07 milliliter implant package, the researchers have packed five customizable biomolecule detectors, along with monitors for pH and temperature. The pH sensor is based on iridium oxide; the thermometer is platinum. Each of the biomolecule sensors is a three-electrode detector whose working electrodes are coated with a special layer comprising chitosan (an antibacterial long-chain sugar often used in implantable devices), multiwall carbon nanotubes, and an enzyme that catalyzes the molecule of interest. The chemical reactions produce current flows within the detector. They are interpreted by a built-in microprocessor (the device is capable of both voltammetric and amperometric analysis) and then transmitted to the power-and-communications patch on the patient’s skin.
Current i-IronIC studies focus on glucose, lactate, glutamate, and adenosine triphosphate (ATP)—all components of the body’s energy production and consumption processes—but the developers say they can produce electrodes that will report for up to a month and a half on a wide range of metabolites.
The DATE 2013 presentations focused on the patch’s power delivery and management system. There are three basic power options for an implanted sensor:
- Implant the power along with the sensor;
- Keep the power pack external and run a wire through the skin to the sensor; or
- Develop wireless power and data transmission.
Wrapping the sensor and the battery up together makes for a bulkier package, and requires surgery for every battery change. Running wires through the skin increases the risk of infection, along with the possibility that wires will snag, causing injury or requiring replacement. A wireless external patch slims the package down, makes it easier to change batteries, and reduces the risk of infection—but it does increase the data-transmission challenges and reduces battery life.
In current tests, the i-IronIC patch’s inductive power link transmitted up to 15 milliwatts through 6 mm of air, and up to 1.17 mW through the experimental surrogate for living tissue—a 17-mm-thick slice of sirloin steak. Under those conditions, battery life is 10 hours on standby or 1.5 hours in operation. (It may come as no surprise that the Bluetooth uplink to the cell phone significantly shortens the operating time.)
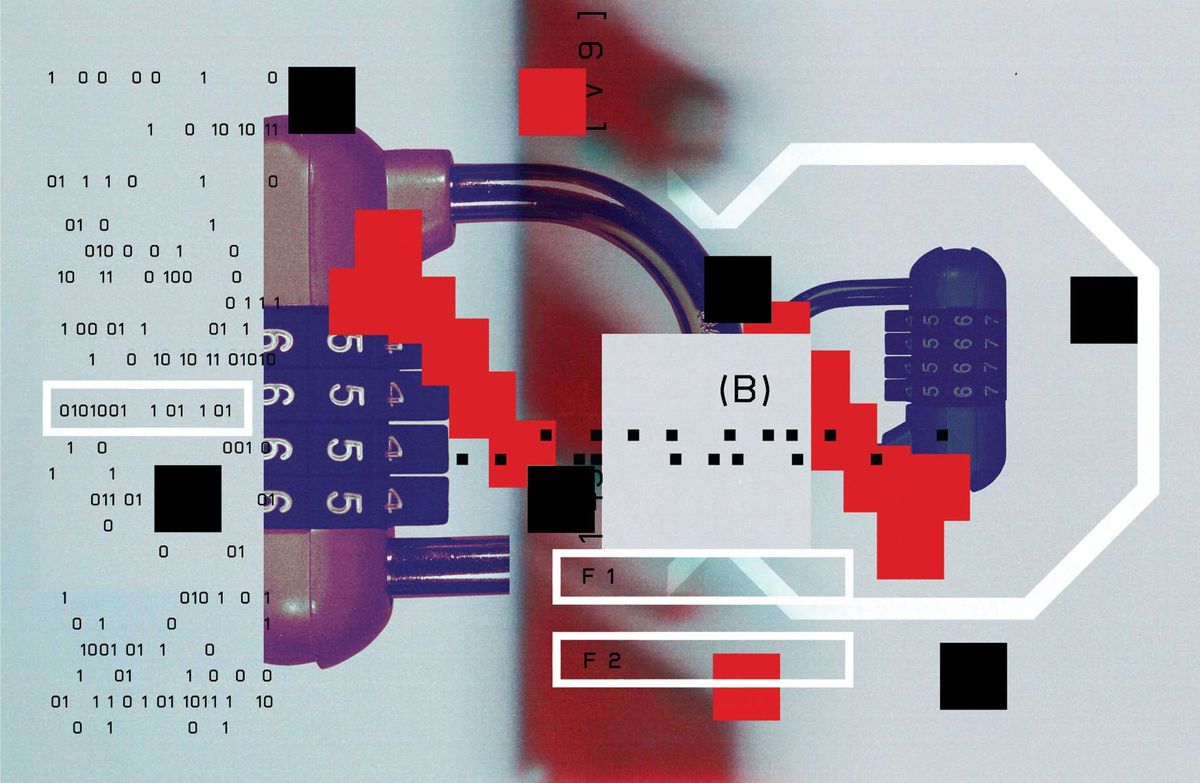
Information is loaded into the implanted chip via amplitude shift keying at 100 kilobits per second. Data moves from chip to patch via a backscatter technique, at 66.6 kb/s. (The uplink is slower because it takes more computing time to double-check the high- and low-current threshold values in real time.) As the researchers point out, backscatter data transmission eliminates the need to include an RF transmitter in the implanted sensor chip.
Douglas McCormick is a freelance science writer and recovering entrepreneur. He has been chief editor of Nature Biotechnology, Pharmaceutical Technology, and Biotechniques.