A few years ago, a report by the New England Healthcare Institute claimed that patients not taking their medications as prescribed incur a staggering US $290 billion in increased medical costs - or about 13 percent of total US health expenditures. Technology reaching drug store shelves later this year in the UK and which is under review in the US could help cut the costs significantly. First, a little background.
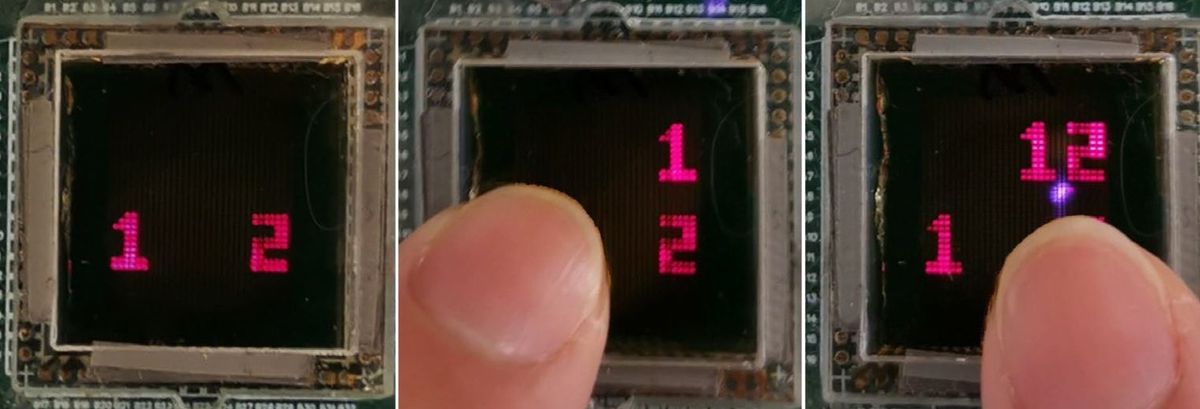
About a year before the Institute's report came out in 2009, there was an article in MIT'sTechnology Review magazine about a Silicon Valley start-up company called Proteus Biomedical that was developing a microchip about the size of a grain of sand called an "ingestible event marker" (IEM). It was to be embedded within a pill and swallowed along with a patient's medicine. The IEM, reported the TR article, consists of:
"... a thin-film battery that is activated on ingestion, as it is exposed to water. The battery, Proteus says, is nontoxic because it is made from materials similar to those in a vitamin pill. Once swallowed, the IEM sends through the body's tissues a high-frequency electrical current that's modulated in such a way that it provides a unique marker of the pill. It's not an RFID technology: it uses the conductive tissues of the body to conduct the signal, rather than a radio, and the signal is confined within the body."
The high-frequency current is picked up by a disposable monitoring patch worn by the patient or a monitor placed under their skin. The monitoring system is able to discern biophysical parameters such as a patient's heart rate, respiration, body posture as well as sleeping patterns. The information can then be transmitted to a patient's cell phone or the computer of the patient's physician. Based on what the physician is seeing, he or she might decided to change dosages or change medications altogether.
Monitoring chemistry-based parameters which would greatly help understand a drug's efficacy is "possible in principle" says the TR article, but that application wasn't what Proteus Biomedical was first targeting.
You can watch the Spectrum video interview with Proteus from December (above). (For more read an October 2011 Spectrum article about wireless technology use in healthcare.)
At the time of the TR article, the company was planning clinical trials in 2009 and hoped to be bringing its "Raisin" system on the market by 2011.
Well, in today's Financial Times of London, there is an article that reports that the UK's Lloydspharmacy chain will be selling pills using the Raisin system in September. The program, called Helius, will "... include a red placebo sugar pill containing a safe and soluble microchip developed by Proteus that patients swallow alongside their existing medicines; an adhesive patch to be changed once a week; and data support." The cost of the monitoring service is slated to be £50 a month.
Currently, the Helius program operates outside the UK's National Health Service (patients wanting it will need to pay for the monitoring capability out-of-pocket). However, the NHS is interested in it for some medical problems such as "... monitoring complex and costly treatments such as organ transplant rejection therapies," the FT reports.
According to a press release at Proteus Biomedical's web site, Lloydspharmacy has 1640 pharmacies in the UK. It also states that Proteus Biomedical is "... developing and commercializing a range of digital health care products in partnership with global leaders from multiple industries, including Novartis, Medtronic, ON Semiconductor, [and] Kaiser Permanente..." in addition to Lloydspharmacy.
The TR article raised a couple of privacy issues (e.g., "... a company wanting to know what medications its prospective employees are taking"), which seemed to focus mainly on ensuring that the information being transmitted from the monitoring system to the patient's call phone or physician's PC wasn't being intercepted (the information from the IEM itself is secure since it isn't transmitted). Proteus Biomedical said that it was confident that it could manage any privacy issue that arose. However, there may be a different type of privacy issue that needs to be thought about assuming the use of the technology becomes widespread, which looks likely.
For example, given the cost of medical prescription non-compliance in the US, I can easily envision a time when this type of technology becomes a mandatory practice, i.e., required by your health insurance company (or your employer who is paying for your insurance or maybe even the U.S. government in the case of Medicare or Medicaid) for getting your prescription covered/reimbursed. And given that the information is being electronically captured, I can also see a point in future where such information automatically becomes part of a person's electronic health record. For those on medications for a long period of time, especially those with mental health issues, such technology could be seen to be pretty intrusive.
Any thoughts on the privacy or security implications of this technology?
Robert N. Charette is a Contributing Editor to IEEE Spectrum and an acknowledged international authority on information technology and systems risk management. A self-described “risk ecologist,” he is interested in the intersections of business, political, technological, and societal risks. Charette is an award-winning author of multiple books and numerous articles on the subjects of risk management, project and program management, innovation, and entrepreneurship. A Life Senior Member of the IEEE, Charette was a recipient of the IEEE Computer Society’s Golden Core Award in 2008.